Articles
- Page Path
- HOME > J Mov Disord > Volume 2(2); 2009 > Article
-
Case Report
A Cerebellar Tremor in a Patient with Human Immunodeficiency Virus-1 Associated with Progressive Multifocal Leukoencephalopathy - Hee-Jin Kim, Jae-Jung Lee, Phil Hyu Lee
-
Journal of Movement Disorders 2009;2(2):88-90.
DOI: https://doi.org/10.14802/jmd.09024
Published online: October 30, 2009
Department of Neurology, Yonsei University College of Medicine, Seoul, Korea
- Corresponding author: Phil Hyu Lee, MD, PhD, Department of Neurology, Yonsei University College of Medicine, 250 Seongsan-ro, Seodaemun-gu, Seoul 120-752, Korea, Tel +82-2-2228-1608, Fax +82-2-393-0705, E-mail phisland@chol.net
• Received: October 7, 2009 • Revised: October 17, 2009 • Accepted: November 8, 2009
Copyright © 2009 The Korean Movement Disorder Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 65,535 Views
- 47 Download
- 2 Crossref
ABSTRACT
- Progressive multifocal leukoencephalopathy (PML) is a demyelinating disease of the central nervous system (CNS) caused by JC virus infection in oligodendrocytes, especially in patients with acquired immunodeficiency syndrome (AIDS). Movement disorders associated with PML are very rare. Here, we report a case of PML in an AIDS patient who presented with a cerebellar tremor, caused by lesions in the cerebellar outflow tract. A cerebellar tremor can be a rare clinical manifestation in patients with PML.
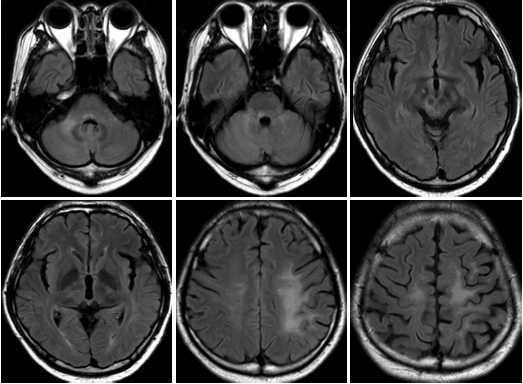
- A previously healthy 34-year-old man visited another university hospital complaining of progressive weakness of the right extremities. The initial imaging findings showed hyper-intensities in the left frontoparietal white matter, right superior cerebellar peduncle, and right posterior pons on fluid-attenuated inversion-recovery (FLAIR) images and hypointensities on T1 images, with no enhancement (Figure 1). A serology work-up to evaluate possible causes of immunocompromise followed. Based on positive laboratory findings in the HIV serology test and typical magnetic resonance imaging (MRI) findings, the patient was diagnosed with presumptive PML, combined with AIDS.2 Efforts to identify JCV DNA in cerebrospinal fluid (CSF) and plasma failed and JCV was detected only in urine by PCR analysis. After beginning highly active antiretroviral therapy (HAART), the number of CD4+ T-cells increased, from 70 to 180 cells/mm3, and negative conversion of HIV RNA copies was noted. However, the weakness of the right extremities slowly worsened. Five months after the initial symptom onset, he felt that his head was shaking and soon after, he developed tremulous movements of the left hand that gradually worsened.
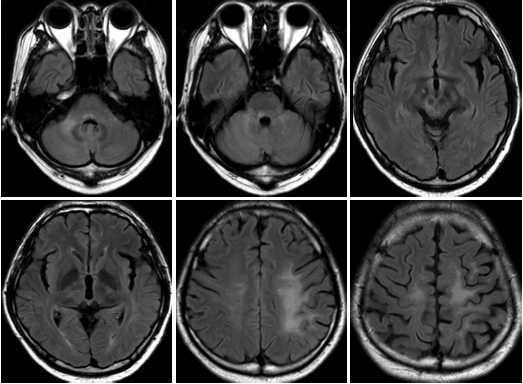
- On admission to our hospital, HIV RNA copies were seen again (41.2/mL) and the CD4+ T-cell count had decreased to 10.2 cells/mm3. The neu-rological examination revealed asymmetric bilateral motor weakness, which was more severe on the right side (IV−) than on the left (IV+). Superficial and deep sensations were preserved. Deep tendon reflexes were hyperactive bilaterally and plan-tar reflexes were extensor bilaterally. When the arms were outstretched, there were large-amplitude, oscillatory, rhythmic movements, with a frequency of 3–4 Hz primarily in the head and left arm. This tremor was augmented on goaldirected movements, while no tremor was seen while resting or sleeping. His higher cognitive functions were unremarkable and his Mini-mental State Examination (MMSE) score was 30. He refused a CSF study to detect JCV DNA. Followup MRI taken 2 months after the onset of the tremor revealed new lesions involving the right thalamus, right retrorubral area, and right posterior pons with extension of the frontoparietal white matter lesions (Figure 2). The introduction of steroid, topiramate (150 mg), and clonazepam (1.5 mg) tended to moderate the amplitude of the tremor.
Case Report
- In patients with HIV-1-associated PML not treated with antiretroviral therapy, the diagnostic sensitivity and specificity of virological analysis of the CSF are 72–92% and 92–100%, respectively.4 Although we failed to detect JCV DNA in the CSF, our patient was compatible with presumptive (clinical) PML, based on the typical clinical and neuroimaging characteristics.2
- The most common presenting signs of PML are hemiparesis or monoparesis, visual defects, language dysfunction, personality changes, and ataxia. The clinical characteristics of PML can be variable, with multiple neurological deficits. Of the rarer combined neurological deficits, several types of movement disorder associated with PML have been reported. Singer, et al.5 reported a patient with PML presenting with a rapidly progressive akinetic-rigid syndrome, while Bhatia, et al.6 reported parkinsonism, combined with cognitive impairments. Others have reported patients with PML presenting with hyperkinetic movement disorders, such as tremor or dystonia.7 Except for one report of very unusual PML by Bhatia, et al., the structural lesions responsible for the movement disorders have been localized to the basal ganglia or areas related to basal ganglia circuits; parkinsonism or dystonia was associated with PML lesions involving in the basal ganglia, whereas tremor was associated with lesions in the cerebellar output pathways.
- Regarding the pathomechanisms of the cerebellar tremor in our patient, the PML lesions involving the midbrain and thalamus could disrupt the contralateral cerebellar outflow pathway, leading to an intention tremor. Similarly, Stockhammer, et al.3 reported a patient with PML presenting with Holmes’ tremor-like phenomenon: a jerky tremor during rest and intentional components during goal-directed movements. Although detailed comparison of the midbrain lesions between our case and the case of Stockhammer, et al. is impossible because of the lack of imaging data, a difference in the involvement of the substantia nigra may lead to different types of tremor.
- In summary, our case illustrates that cerebellar tremor can be a rare clinical manifestation in patients with PML.
Discussion
Figure 1.The initial MRI shows multifocal lesions involving in left frontoparietal white matter, right superior cerebellar peduncle, and right posterior pons on fluid-attenuated inversion recovery images.
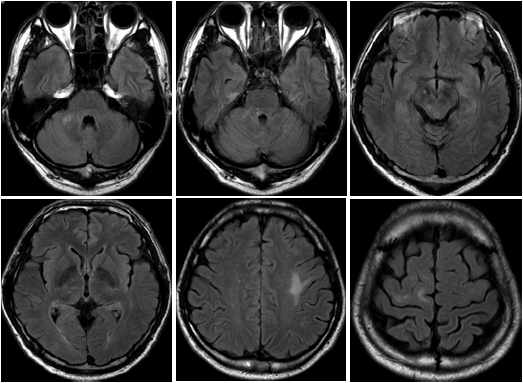
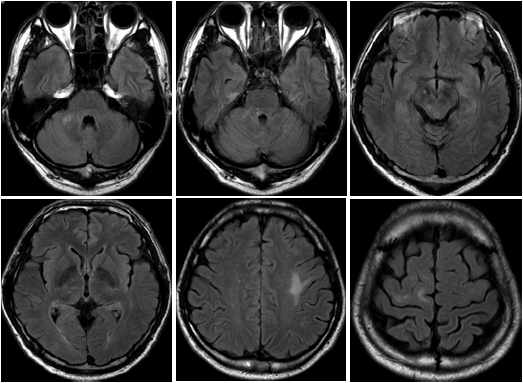
Figure 2.A follow-up MRI taken 2 months after onset of the tremor revealed new lesions involving the right thalamus, right retrorubral area, and right posterior pons with extension of the frontoparietal white matter lesions.
- 1. Richardson EP Jr. Progressive multifocal leukoencephalopathy. N Engl J Med 1961;265:815–823.ArticlePubMed
- 2. Cinque P, Koralnik IJ, Gerevini S, Miro JM, Price RW. Progressive multifocal leukoencephalopathy in HIV-1 infection. Lancet Infect Dis 2009;9:625–636.ArticlePubMedPMC
- 3. Stockhammer G, Poewe W, Wissel J, Kiechl U, Maier H, Felber S. Progressive multifocal leukoencephalopathy presenting with an isolated focal movement disorder. Mov Disord 2000;15:1006–1009.ArticlePubMed
- 4. Cinque P, Scarpellini P, Vago L, Linde A, Lazzarin A. Diagnosis of central nervous system complications in HIV-infected patients: cerebrospinal fluid analysis by the polymerase chain reaction. AIDS 1997;11:1–17.ArticlePubMed
- 5. Singer C, Berger JR, Bowen BC, Bruce JH, Weiner WJ. Akinetic-rigid syndrome in a 13-year-old girl with HIV-related progressive multifocal leukoencephalopathy. Mov Disord 1993;8:113–116.ArticlePubMed
- 6. Bhatia KP, Morris JH, Frackowiak RS. Primary progressive multifocal leukoencephalopathy presenting as an extrapyramidal syndrome. J Neurol 1996;243:91–95.ArticlePubMed
- 7. Rieder CR, Ziomkowski SC. Head tremor and progressive multifocal leukoencephalopathy in AIDS patients: report of two cases. Arq Neuropsiquiatr 2005;63:150–153.ArticlePubMed
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

- Holmes tremor in progressive multifocal leukoencephalopathy: A video case report
Takako Matsushima, Ryotaro Ikeguchi, Mutsumi Iijima, Ayato Shimomura, Shuntaro Takahashi, Kazuo Nakamichi, Yuko Shimizu, Kazuo Kitagawa
Clinical and Experimental Neuroimmunology.2023;[Epub] CrossRef - Holmes tremor caused by a natalizumab-related progressive multifocal leukoencephalopathy: a case report and brief review of the literature
Luca Magistrelli, Domizia Vecchio, Paola Naldi, Cristoforo Comi, Roberto Cantello
Neurological Sciences.2019; 40(9): 1943. CrossRef
Comments on this article
 KMDS
KMDS
 E-submission
E-submission
 PubReader
PubReader ePub Link
ePub Link Cite
Cite


