Articles
- Page Path
- HOME > J Mov Disord > Volume 17(2); 2024 > Article
-
Letter to the editor
Meige Syndrome as a Craniofacial Type of Dystonia Treatable by Dual Dopaminergic Modulation Using L-DOPA/Chlorpromazine: A Case Report -
Shinichi Matsumoto1
 , Satoshi Goto2,3
, Satoshi Goto2,3

-
Journal of Movement Disorders 2024;17(2):233-235.
DOI: https://doi.org/10.14802/jmd.23265
Published online: January 23, 2024
1Department of Neurology, Osaka Neurological Institute, Osaka, Japan
2Center for Drug Discovery and Development Sciences, Research Organization of Science and Technology, Ritsumeikan University, Kyoto, Japan
3Department of Clinical Neuroscience, Institute of Biomedical Sciences, Tokushima University, Tokushima, Japan
- Corresponding author: Satoshi Goto, MD, PhD Center for Drug Discovery and Development Sciences, Research Organization of Science and Technology, Ritsumeikan University, 56-1 Tojiin Kitamachi, Kita Ward, Kyoto 603-8577, Japan / Tel: +81-077-561-2802 / Fax: +81-077-561-2811 / E-mail: sgoto0326@outlook.jp
Copyright © 2024 The Korean Movement Disorder Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 346 Views
- 42 Download
- Dear Editor,
- Meige syndrome [1] is an adult-onset craniofacial dystonia characterized by the combination of blepharospasm and oromandibular dystonia [2]. It can be a primary (idiopathic) or parkinsonian condition [2]. Among the symptomatic therapies, the peripheral application of botulinum toxins (BTXs) is currently considered the most effective treatment for Meige syndrome [2], but its therapeutic efficacy varies and is not long-lasting. In clinical practice, treating Meige syndrome with conventional therapeutic tools is often difficult. It has been hypothesized that imbalanced activities between dopamine D1- and D2-type receptors (D1Rs and D2Rs) in the striatum might cause repetitive stereotyped motor symptoms, which are the key features of dystonia [3-5]. Here, we report the striking and long-lasting benefits of dual dopaminergic modulation (DDM) via the use of L-DOPA and chlorpromazine (CPZ) [4,5] in a patient with idiopathic Meige syndrome who poorly responded to BTX treatment.
- A 73-year-old woman experienced gradual onset and worsening of blepharospasm and oromandibular dystonia beginning at age 67. She had no prior exposure to neuroleptics and no family history of dystonia. She had no history of alcohol consumption or smoking. Upon admission, she exhibited marked facial grimacing with excessive blinking or sustained forceful eye closure in combination with forced contractions of the jaw and tongue muscles, leading to difficulty in opening the mouse to speak and eat. Severe spasmodic dysphonia was also observed. All dystonia symptoms were sustained throughout the day and were exacerbated by emotional and physical stresses. Physical examinations revealed no cranial nerve abnormalities or overt parkinsonism. Brain MRI showed no obvious abnormalities. Laboratory testing revealed no abnormalities, and no pathogenic variants in the known dystonia genes were identified by whole-exome sequencing (OMIM Phenotypic Series PS128100; https://omim.org/phenotypicSeries/PS128100). Thus, she was diagnosed with idiopathic Meige syndrome.
- Oral medication with lorazepam, etizolam, loflazepate, or paroxetine was not beneficial. She refused to take anticholinergics because of possible cognitive decline. Accordingly, she received a total of 100 units of BotoxTM, which was injected bilaterally into the orbicularis oculi (25 units), orbicularis oris (20 units), corrugator (5 units), masseter (10 units), and platysma (40 units) muscles. However, this BTX treatment did not achieve any satisfactory results at the 3-month follow-up.
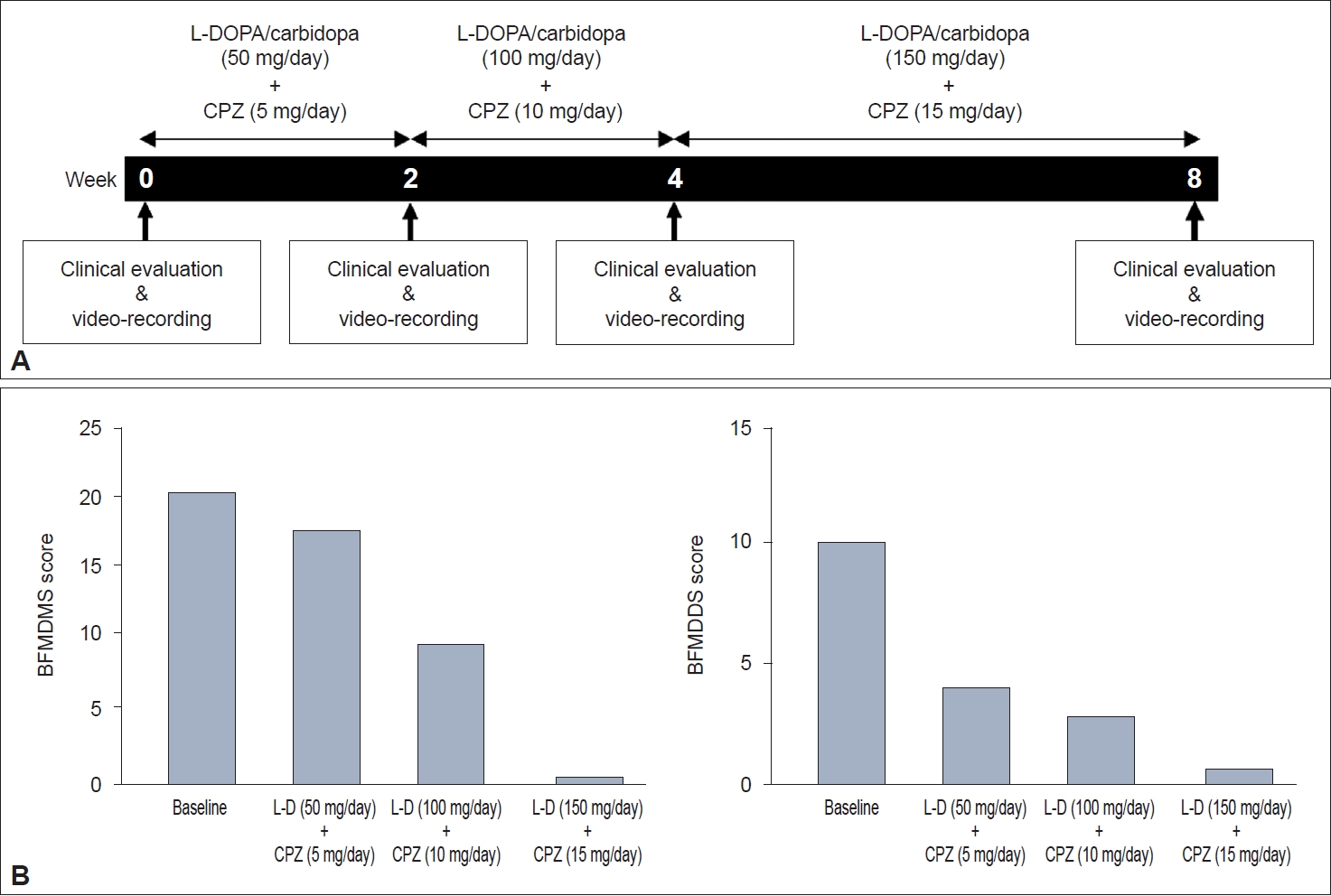
- She then underwent DDM using L-DOPA and CPZ. Before the treatment, her Burke-Fahn-Marsden Dystonia Movement Scale (BFMDMS) [6] and Dystonia Disability Scale (BFMDDS) [6] scores were 20 (maximum 120) and 10 (maximum 30), respectively. As shown in Figure 1A, daily doses of L-DOPA/carbidopa and CPZ-phenolphthalinate were increased stepwise up to 150 mg/day and 15 mg/day, respectively, over 8 weeks [4,5]. Clinical evaluation and video recording were performed 1 day before (baseline) and 2, 4, and 8 weeks after drug initiation. As a result, DDM using L-DOPA and CPZ attenuated her dystonia symptoms in a dose-related manner (Figure 1B, Supplementary Video 1 in the online-only Data Supplement). When L-DOPA/carbidopa (150 mg/day) and CPZ-phenolphthalinate (15 mg/day) were used, her blepharospasm and oromandibular dystonia were almost completely resolved (Supplementary Video 1 in the online-only Data Supplement). Complete remission of spasmodic dysphonia was also observed. Her BFMDMS and BFMDDS scores were 1 and 1, respectively (Figure 1B). This striking benefit obtained with DDM using DOPA/carbidopa (150 mg/day) and CPZ-phenolphthalinate (15 mg/day) remains unchanged at the time of this writing, which is more than one year after treatment. No adverse effects have been observed thus far.
- In our patient with idiopathic Meige syndrome, all aspects of dystonia symptoms could be markedly alleviated by DDM using L-DOPA and CPZ (L-DOPA/CPZ) at doses lower than those used in the clinic. Since L-DOPA is a D1/D2 agonist and CPZ is a D2 antagonist, her dystonia symptoms might be alleviated through DDM, which induces an increase in D1 signaling with a relative decrease in D2 signaling in the striatum.
- The key features of dystonia are characterized by repetitive and stereotyped motor symptoms [3-5]. It is hypothesized that repetitive stereotyped motor and cognitive symptoms might be due to the altered function of a neural circuit connecting the prefrontal cortex with the striatal “striosomes”, which participate in reinforcement-related learning and decision-making under conflict [7]. This hypothesis implies that the output activity of the cortico-striatal (striosomal) network, which receives afferent signals through the monosynaptic and/or multisynaptic pathways arising from various brain regions, such as the thalamus, cerebellum, and brainstem, is important in considering dystonia pathology and treatment. Corticostriatal inputs are largely integrated by striatal medium spiny neurons (MSNs), which constitute the vast majority of striatal neurons and constitute the major striatal efferent system in basal ganglia circuits [7].
- Deregulation of striatal dopamine signaling is a potential cause of dystonia [4,5]. The loss of dopamine D1 signaling in striatal striosomes has been proposed to be an important pathology that induces dystonia [3-5]. A modular computational model of the basal ganglia circuits suggested that striosomal D1 signaling participates in the representation of motor action selection (or focusing) and that its impairments cause stereotyped motor symptoms [3]. This assumption is relevant to the functional pathology of several human disease models of dystonia, such as DYT25 and DYT3 (X-linked dystonia-parkinsonism) [4]. It is thus conceivable that striosomal loss of D1 signaling underlies the dystonia manifestation in Meige syndrome patients.
- The specificity of the striatal dopamine D1 system in humans [8] is the neural basis for the therapeutic mechanism of DDM using low doses of L-DOPA/CPZ for the treatment of idiopathic dystonia [4,5]. The human neostriatum exhibits a pronounced enrichment of D1Rs in the striosomal MSNs but a relative paucity of D1Rs in the matrix MSNs [8]. These findings suggest that a low dose of L-DOPA could exert its D1-agonistic effects primarily on striosomal MSNs. We thus believe that DDM using low doses of L-DOPA/CPZ could improve dystonia symptoms by increasing striosomal D1-activity [4,5]. Moreover, the concurrent use of CPZ may strengthen the D1-agonistic effect of L-DOPA on the striosomal network in a synergistic manner [4,5].
- In conclusion, DDM using low doses of L-DOPA/CPZ could exert a striking and long-lasting therapeutic effect on patients with idiopathic Meige syndrome refractory to BTX treatment. Since DDM therapy has also been effective for idiopathic blepharospasm [4] and cervical dystonia [5], further investigations of this treatment modality for a wide spectrum of idiopathic dystonia, including Meige syndrome, may be warranted.
Supplementary Materials
Video 1.
-
Ethics Statement
This clinical study was approved by the Institutional Ethics Committee of Osaka Neurological Institute (reference number: OR01-4). Informed consent from the patient is obtained. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this work is consistent with those guidelines. The study was registered with an International Committee of Medical Journal Editors recognized registry, the UMIN Clinical Trials Registry (UMIN000027430).
-
Conflicts of Interest
The authors have no financial conflicts of interest.
-
Funding Statement
None
-
Author Contributions
Conceptualization: Satoshi Goto. Data curation: Shinichi Matsumoto. Formal analysis: Shinichi Matsumoto. Funding acquisition: Satoshi Goto. Investigation: Shinichi Matsumoto. Methodology: Shinichi Matsumoto. Project administration: Satoshi Goto. Resources: Satoshi Goto. Software: Satoshi Goto. Supervision: Satoshi Goto. Validation: Satoshi Goto. Visualization: Shinichi Matsumoto. Writing—original draft: Shinichi Matsumoto. Writing—review & editing: Satoshi Goto.
Notes
- The authors acknowledge and thank Dr. Kenichi Amemori of Kyoto University for his helpful comments and suggestions in working out the design of this research project.
Acknowledgments
- 1. Meige H. [Les convulsions de la face: une forme clinique deconvulsion faciale, bilatérale et médiane]. Rev Neurol (Paris) 1910;10:437–443.French.
- 2. Pandey S, Sharma S. Meige’s syndrome: history, epidemiology, clinical features, pathogenesis and treatment. J Neurol Sci 2017;372:162–170.ArticlePubMed
- 3. Amemori K, Gibb LG, Graybiel AM. Shifting responsibly: the importance of striatal modularity to reinforcement learning in uncertain environments. Front Hum Neurosci 2011;5:47.ArticlePubMedPMC
- 4. Matsumoto S, Koizumi H, Shimazu H, Kaji R, Goto S. A dual dopaminergic therapy with L-3,4-dihydroxyphenylalanine and chlorpromazine for the treatment of blepharospasm, a focal dystonia: possible implications for striosomal D1 signaling. Front Neurol 2022;13:922333.Article
- 5. Matsumoto S, Koizumi H, Shimazu H, Goto S. Therapeutic effects of dual dopaminergic modulation with L-DOPA and chlorpromazine in patients with idiopathic cervical dystonia. Neurol Clin Pract 2024;14:e200254. PubMed
- 6. Burke RE, Fahn S, Marsden CD, Bressman SB, Moskowitz C, Friedman J. Validity and reliability of a rating scale for the primary torsion dystonias. Neurology 1985;35:73–77.ArticlePubMed
- 7. Graybiel AM, Matsushima A. Striosomes and matrisomes: scaffolds for dynamic coupling of volition and action. Annu Rev Neurosci 2023;46:359–380.ArticlePubMed
- 8. Goto S. Specificity of striatal dopamine D1 system in humans: implications for clinical use of D1 receptor-agonists in Parkinson’s disease. Front Hum Neurosci 2023;17:1178616.ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

Comments on this article
 KMDS
KMDS
 E-submission
E-submission
 PubReader
PubReader ePub Link
ePub Link Cite
Cite

