Articles
- Page Path
- HOME > J Mov Disord > Volume 13(2); 2020 > Article
-
Original Article
Association between Olfactory Deficit and Motor and Cognitive Function in Parkinson’s Disease -
Han Soo Yoo1
 , Seok Jong Chung1
, Seok Jong Chung1 , Yang Hyun Lee1, Byoung Seok Ye1
, Yang Hyun Lee1, Byoung Seok Ye1 , Young H. Sohn1
, Young H. Sohn1 , Phil Hyu Lee1,2
, Phil Hyu Lee1,2
-
Journal of Movement Disorders 2020;13(2):133-141.
DOI: https://doi.org/10.14802/jmd.19082
Published online: April 6, 2020
1Department of Neurology, Yonsei University College of Medicine, Seoul, Korea
2Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul, Korea
- Corresponding author: Phil Hyu Lee, MD, PhD Department of Neurology, Yonsei University College of Medicine, 50 Yonsei-ro, Seodaemun-gu, Seoul 03722, Korea / Tel: +82-2-2228-1608 / Fax: +82-2-393-0705 / E-mail: phlee@yuhs.ac
Copyright © 2020 The Korean Movement Disorder Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objective
- To investigate whether baseline olfactory dysfunction in Parkinson’s disease (PD) patients is associated with baseline and longitudinal motor and cognitive function.
-
Methods
- We recruited 228 drug-naïve PD patients who were followed for a mean of 6 years. Patients underwent the Cross-Cultural Smell Identification Test (CCSIT), a neuropsychological test, and N-(3-[18F]fluoropropyl)-2β-carbomethoxy-3β-(4-iodophenyl) nortropane positron emission tomography within 6 months of the baseline evaluation. Olfactory dysfunction was categorized as normosmia (CCSIT score ≥ 9), hyposmia (CCSIT score 5–8), and anosmia (CCSIT score ≤ 4). During the follow-up period, we investigated changes in the levodopa-equivalent dose (LED) and the occurrence of wearing-off, levodopa-induced dyskinesia, and dementia.
-
Results
- Among the PD patients, 80.7% were hyposmic at the time of diagnosis, and 26.1% were anosmic. Baseline olfactory dysfunction was not associated with either initial parkinsonian motor symptoms or with the longitudinal LED increment and motor complications. Meanwhile, the anosmic group had lower baseline scores on the Korea version of the Boston Naming Test and Stroop color reading test than the normosmic and hyposmic groups. The anosmic group exhibited a higher rate of conversion to dementia than the normosmic [adjusted hazard ratio (HR) 3.99, 95% confidence interval (CI) 1.08–14.72] and hyposmic (adjusted HR 2.48, 95% CI 1.15–5.32) PD groups, regardless of baseline motor deficits and cognitive status.
-
Conclusion
- Baseline olfactory dysfunction was not associated with motor deficits and complications, but it was associated with cognitive dysfunction and prognosis, suggesting that severe olfactory impairment may reflect early cortical involvement, probably in the frontotemporal region, and rapid spreading of Lewy body pathology.
- Study participants
- In this retrospective cohort study, we consecutively recruited 228 drug-naïve patients with PD who visited the movement disorders outpatient clinic at Severance Hospital, Yonsei University Health System, from June 2009 to March 2016; all included patients has been followed for at least three years and up to 10 years. All subjects had undergone neurological examination, UPDRS, Cross-Cultural Smell Identification Test (CCSIT), neuropsychological test, brain magnetic resonance imaging (MRI), and N-(3-[18F]fluoropropyl)-2β-carbomethoxy-3β-(4-iodophenyl) nortropane (18F-FP-CIT) PET within six months. The diagnosis of PD was based on the clinical diagnostic criteria of the United Kingdom PD Society Brain Bank. All patients with PD showed decreased DAT uptake in the posterior putamen and responded to dopaminergic medication. RBD was assessed with the RBD Screening Questionnaire. The LED was calculated according to a previously described method [12]. We excluded patients with severe white matter hyperintensities; multiple lacunes in the basal ganglia or hydrocephalus on MRI; other neurologic, psychiatric, or metabolic illnesses; dementia at baseline evaluation; atypical parkinsonism such as multiple system atrophy, corticobasal degeneration, or progressive supranuclear palsy; or any conditions affecting olfactory function, including history of nasal surgery, chronic sinonasal disease, recent upper respiratory tract infections, or major head trauma.
- This study was approved by the Institutional Review Board of Yonsei University Severance Hospital (IRB No. 4-2014-0637). Given the retrospective nature of the present study, written informed consent was waived.
- Assessment of olfactory function and grouping according to olfactory function
- Olfactory function was assessed with the CCSIT, which consists of 12 odors [13]. Participants were required to scratch the panel, sniff the sample, and select from one of four possible answers. Their scores were calculated as the sum of correct responses. Based on previous studies, normosmia was diagnosed when the score ranged from 9 to 12, hyposmia was diagnosed when the score ranged from 5 to 8, and anosmia was diagnosed when the score ranged from 0 to 4 [14].
- PET image acquisition
- 18F-FP-CIT PET scans were obtained using a Discovery 600 system (General Electric Healthcare, Milwaukee, MI, USA). A dose of 185 MBq (5 mCi) of 18F-FP-CIT was injected intravenously during the procedure. Ninety minutes after the injection, images were acquired during a 20-minute session, followed by a CT scan for attenuation correction. The spiral CT scan was performed with a 0.8 s/rotation at 120 kVp, 10 mA, 3.75 mm slice thickness, 0.625 mm collimation and 9.375 mm table feed per rotation. Images were reconstructed using the ordered subset expectation maximization algorithm with ƒ iterations and 32 subsets. A Gaussian filter with a full-width at half-maximum of 4 mm was applied to each reconstructed PET image, which was made up of a 256 × 256 matrix with 0.98 mm pixel and 0.98 mm slice thickness.
- Quantitation of the 18F FP-CIT PET-CT images
- We analyzed the 18F-FP-CIT PET images according to the method described in a previous study [15]. Image processing was performed using Statistical Parametric Mapping 8 (Wellcome Department of Imaging Neuroscience, Institute of Neurology, University College London, London, UK) with MATLAB R2013a for Windows (Math Works, Natick, MA, USA). Quantitative analyses were based on the volumes of interest (VOIs), which were defined based on a template in standard space. All reconstructed PET images were spatially normalized to Talairach space by using a standard 18F-FP-CIT PET template, which was made inhouse, as described previously [16]. Four VOIs of the bilateral caudate nuclei and putamen and one occipital VOI were drawn on a coregistered spatially normalized single T1 MRI and 18F-FPCIT PET template image on MRIcro version 1.37 (Chris Rorden, Columbia, SC, USA). These VOIs were adjusted by minor translation using our in-house editing software, ANIQUE (Department of Nuclear Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea). The level of DAT activity in each VOI was calculated in terms of the specific to non-specific binding ratio as follows: (mean standardized uptake of the striatal subregional VOI-mean standardized uptake of the occipital VOI)/mean standardized uptake of the occipital VOI. For non-specific binding, the mean standardized uptake value was calculated by drawing two occipital VOIs, one on each side.
- Clinical parameters and assessment of motor function
- At baseline, parkinsonian motor symptoms were assessed during a drug-naïve state at the time of 18F-FP-CIT PET acquisition using the UPDRS motor (UPDRS-III) subscales. Tremor and non-tremor scores were calculated in each patient according to a previously described method, and patients were classified into three clinical subtypes: tremor-dominant, akinetic-rigid, and mixed [17]. DAT activity in the putamen was used to evaluate striatal function in relation to parkinsonian motor function.
- We investigated longitudinal changes in the dose of dopaminergic medication using the LED during the first three years of follow-up, which can indirectly reflect the progression of parkinsonian motor symptoms. We also assessed the occurrence of motor complications, including wearing-off (WO) and levodopainduced dyskinesia (LID), during the follow-up period. Patients with PD visited the outpatient clinic every three to six months, and two movement disorders experts (Y.H.S. and P.H.L.) carefully examined them for the presence of motor complications based on the patient history provided by the patients and their caregivers or by performing direct neurological examination at every visit. We considered the date on which the PD patients or their caregivers reported the occurrence of motor complications or the date on which motor complications were first observed in the clinic as the date of the occurrence of motor complications.
- Clinical parameters and assessment of cognitive function
- At baseline, all participants underwent a standardized neuropsychological battery called the Seoul Neuropsychological Screening Battery [18], which is composed of the following scorable tests: digit span (forward and backward), repetition, the Korean version of the Boston Naming Test (K-BNT), the 6-point pentagon drawing test, the Rey-Osterrieth Complex Figure Test (copying, immediate and 20-min delayed recall, and recognition), the Seoul Verbal Learning Test (SVLT; immediate recall, 20-min delayed recall, and recognition), contrasting programming and the go/no-go test, the clock drawing test, the phonemic and semantic Controlled Oral Word Association Test, the Stroop Test (word and color reading), the Korean version of the Mini-Mental State Examination (K-MMSE), and the Clinical Dementia Rating. Each score was converted into a standardized score (z-score) based on age- and education-specific norms. Patients were diagnosed with PD with intact cognition when impairments were observed in less than two items on the detailed neuropsychological tests. In accordance with the Movement Disorder Society Task Force guidelines, a diagnosis of PD with mild cognitive impairment (MCI) was made when there was no evidence of abnormal activities in daily living (ADLs). DAT activity in the caudate was used to assess striatal function in relation to cognitive function.
- PD patients were followed-up for more than three years, and they performed neuropsychological tests or the K-MMSE every two to three years or when they or their caregivers complained of cognitive decline in their daily living activities. Patients were diagnosed with PD with dementia if they fulfilled the clinical criteria for probable PD with dementia based on the Movement Disorder Society Task Force guideline (both level I and II testing) with evidence of abnormal ADLs. Impairment of cognitive decline in ADLs was assessed both clinically and with the ADL scale.
- Statistical analyses
- The baseline demographic characteristics of the study participants were analyzed using the independent t-test or Pearson χ2-test as appropriate. To compare baseline motor and cognitive parameters, we performed analysis of covariance (ANCOVA) using age, sex, and the interval from PD onset to CCSIT evaluation as covariates for continuous variables, and we performed the Pearson χ2-test for categorical variables. Partial correlation analysis was performed to investigate the correlation between the CCSIT score and neuropsychological performance. Corrections for multiple analyses across 15 neuropsychological items were performed using the false discovery rate (FDR) method in the ANCOVA and partial correlation analyses. A linear mixed model was used to examine the differences in the rates of longitudinal changes in the LED among the groups after controlling for the same covariates. The effects of the PD subgroups on changes in the LED over time were tested using the time by PD subgroup interaction term. To investigate the hazard ratio (HR) of developing WO, LID, or conversion to dementia, we used a Cox proportional hazards model that included the same covariates. We further adjusted for the total UPDRS-III score and cognitive status in the Cox proportional hazards model for conversion to dementia according to olfactory dysfunction. Data were analyzed using SPSS software, ver. 23 (IBM Corp., Armonk, NY, USA). p-values less than 0.05 were considered significant.
MATERIALS & METHODS
- Demographic and clinical characteristics of the study participants
- According to the baseline CCSIT scores, 19.3% of PD patients had normal olfactory function, 59.6% had mildly decreased olfaction, and 21.1% had severe olfactory loss at the time of PD diagnosis (Table 1). Anosmic PD patients were older at PD onset, and a higher proportion of these patients were male compared to the normosmic and hyposmic PD groups. The interval from PD onset to CCSIT evaluation, follow-up duration, total disease duration, and proportion of RBD were not different among the groups.
- Baseline motor profiles of the study participants
- The baseline parkinsonian motor score and DAT activity in the putamen were not different among the PD groups after controlling for age, sex, and the interval from PD onset to CCSIT evaluation (Table 2). There was also no difference in the proportion of clinical subtypes among the PD groups.
- Baseline cognitive profiles of the study participants
- At the baseline neuropsychological evaluation, the anosmic PD group had a higher proportion of MCI than the normosmic PD group (Table 2). There was no difference in the proportion of patients with amnestic MCI among the PD groups. Among the neuropsychological battery of tests, the anosmic PD patients showed significantly poorer performance on the K-BNT (p = 0.005) and Stroop color reading (p = 0.023) items when uncorrected. Additionally, we investigated the association between olfactory function and neuropsychological performance using the CCSIT as a continuous variable. The CCSIT score was significantly correlated with the K-BNT, Stroop color reading, and SVLT recognition scores after applying the FDR method (Supplementary Table 1 in the online-only Data Supplement). The three PD groups showed no differences in any of the other neuropsychological tests or in the DAT activity in the caudate.
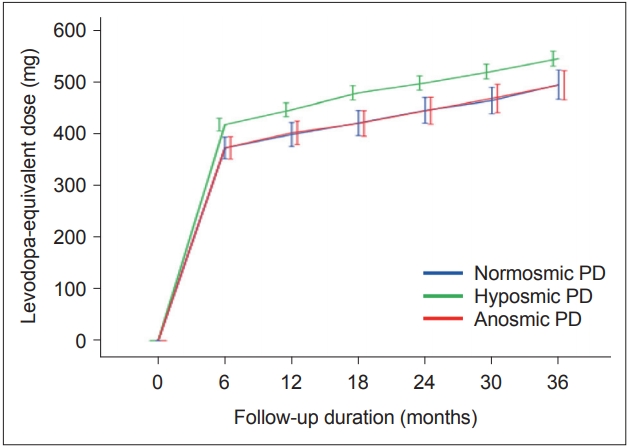
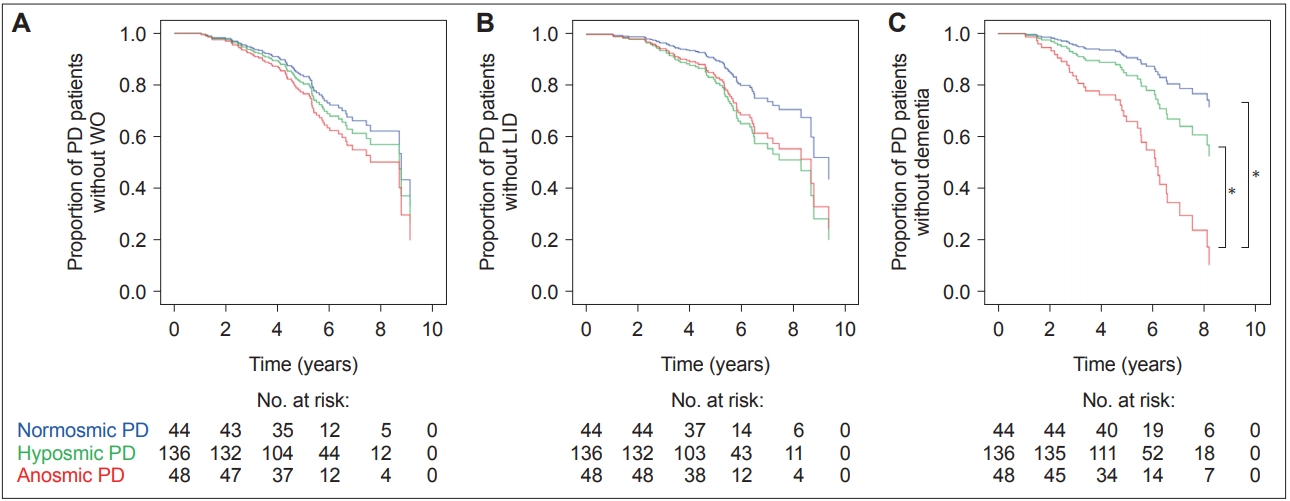
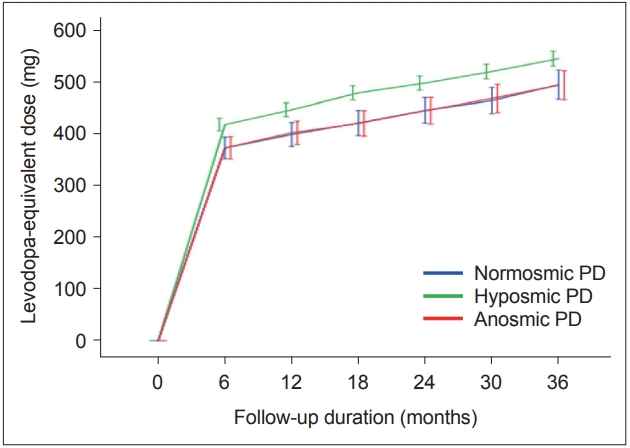
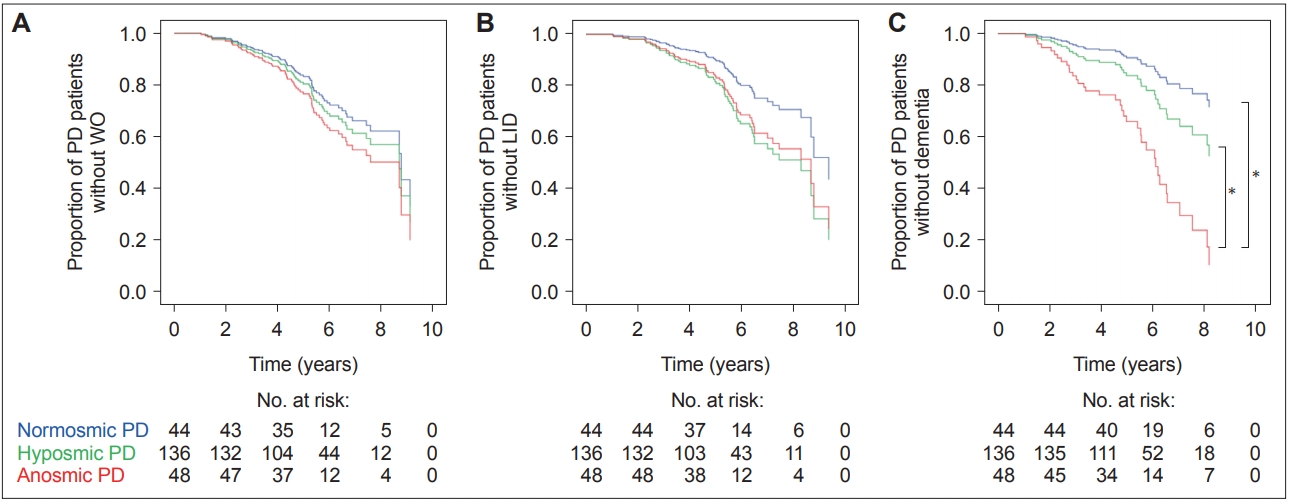
- Longitudinal changes in the LED and occurrence of motor complications
- A linear mixed model analysis showed that there were no differences in the rate of LED changes during the first three years of follow-up among the PD groups (time by PD subgroup interaction, p = 0.144) (Figure 1). A Cox proportional hazard model according to olfactory dysfunction in PD patients showed no difference in the occurrence of WO (Figure 2A) and LID (Figure 2B) among the PD groups.
- Occurrence of PD dementia
- The anosmic PD group showed a significantly higher conversion rate to dementia than the normosmic [HR 3.89, 95% confidence interval (CI) 1.06–14.21] and hyposmic (HR 2.20, 95% CI 1.04–4.66) PD groups, independent of age, sex, and interval from PD onset to CCSIT evaluation (Figure 2C, Table 3). When we further adjusted for the total UPDRS-III score and cognitive status, the anosmic group still had a higher conversion rate to dementia than the normosmic (HR 3.99, 95% CI 1.08–14.72) and hyposmic (HR 2.48, CI 1.15–5.32) PD groups. Additionally, we investigated the HR of olfactory dysfunction for dementia conversion using the CCSIT as a continuous variable. The HR of the baseline CCSIT score for the risk of future development of dementia was 0.73 (95% CI 0.61–0.87) after controlling for age, sex, interval from PD onset to CCSIT evaluation, total UPDRS-III score, and cognitive status.
RESULTS
- The present study investigated the association of baseline olfactory function with motor and cognitive deficits and the longitudinal motor and cognitive outcomes in PD. The major findings were as follows: 1) 81.1% of PD patients had decreased olfaction at the time of diagnosis, and 26.1% of PD patients had severe loss of olfaction; 2) olfactory dysfunction was not associated with initial parkinsonian motor symptoms but was associated with baseline dysfunction in the K-BNT and Stroop color reading test, which reflect deficits in frontal and temporal functions; 3) baseline olfactory dysfunction was neither associated with motor progression nor with the occurrence of motor complications; and 4) baseline olfactory dysfunction predicted the progression to dementia regardless of baseline motor deficits and cognitive status. Taken together, these results suggest that, while baseline olfactory dysfunction is not associated with motor deficits and complications, it is associated with cognitive dysfunction and prognosis.
- Severely decreased olfaction at the time of PD diagnosis was associated with MCI and poor performance in the K-BNT and Stroop color reading test. Previous studies reported that PD patients with MCI have worse olfactory function than those with intact cognition [9,19,20]. This suggests the early involvement of the cortical Lewy body, a pathological hallmark of PD, in cases where there is initiation of neuropathological spread of the neurodegenerative process through an olfactory route [21]. However, heterogeneous results have been reported regarding which specific cognitive domain is impaired in association with olfactory dysfunction in PD: attentional deficit [10], visuospatial dysfunction [19], memory impairment [22-24], or executive dysfunction [22,24]. This can be attributed to the different ways of evaluating olfactory and cognitive functions and to studies that enrolled PD patients with various disease stages. Since antiparkinsonian drugs have the potential to influence a range of cognitive functions, it is necessary to investigate the association between olfactory and cognitive functions in early and drug-naïve PD patients. Furthermore, as we enrolled PD patients with a mean disease duration of less than 2 years at baseline evaluation, we can infer that, from the early stage of PD, olfactory deficits are closely related to specific cognitive dysfunction, and they are predictive of future development of dementia. Imaging studies have revealed that olfactory dysfunction is associated with olfaction-related cortical atrophy, including piriform and orbitofrontal cortices [25] or white matter disintegrity near the orbitofrontal cortex in PD [20]. Since olfactionrelated structures are located near and within the basal and medial frontal regions and the inferior and medial temporal areas, Lewy body entry through the nasal route could primarily affect these regions from the early stage of PD [21]. The suggested neural correlate involved in naming is the inferior temporal cortex [26] and that of the Stroop color reading test is the prefrontal cortex [27]. From our results, we can infer that baseline olfactory dysfunction is closely linked to the early presence of Lewy bodies in the frontotemporal regions, which leads to dysfunction in naming and frontal execution in PD. Pathological studies are necessary to investigate the timing and preferential site for cortical involvement of Lewy bodies according to olfactory dysfunction.
- We found that PD patients with severe olfactory dysfunction at the time of PD diagnosis had a higher rate of conversion to dementia than other PD patients, independent of age, sex, and baseline motor and cognitive functions. Consistent with our study, previous studies have reported that baseline hyposmia in PD patients is an independent risk factor for the subsequent development of MCI [6] and dementia [3]. Additionally, PD patients with baseline hyposmia had a characteristic cerebral metabolic decline that was identical to that in PD dementia [8]. Olfactory dysfunction was also closely associated with cognitive decline, even in dementia-free subjects [28] and in patients with amnestic MCI and Alzheimer’s disease (AD) [29]. Worse olfaction may reflect early and severe extranigral Lewy body pathology in the cortical areas, which could accelerate the progression of cognitive decline and conversion to dementia [6]. Early damage to the forebrain cholinergic system could be another explanation for the association between olfactory dysfunction and cognitive decline. Patients with PD show substantial neuronal loss in the nucleus basalis of Meynert [30]. Odor identification test scores have been shown to be positively correlated with acetylcholinesterase activity in the limbic area [23]. PET studies have revealed widespread and profound cholinergic dysfunction in PD dementia [31]. If we can identify a temporal relationship between olfactory impairment and cholinergic dysfunction, it will enable us to elucidate the role of olfactory dysfunction in cognitive decline. Last, co-accumulation of AD neuropathologies such as amyloid plaque and neurofibrillary tangles can link olfactory dysfunction and cognitive decline. Tau-related pathology has been found in the anterior olfactory nucleus in PD [32]. Olfactory impairment has been shown to be associated with atrophy in AD signature areas in dementia-free older adults [33]. Concomitant AD neuropathologies have been found to be associated with rapid cognitive decline in Lewy body disorders [34]. Since patients in the anosmic PD group in this study had a higher age of onset and proportion of MCI than the other groups, AD co-pathology may have accelerated cognitive decline and dementia conversion in the anosmic PD group. It is necessary to investigate the burden of amyloid-β burden according to the baseline olfactory function in PD.
- Olfactory dysfunction was not associated with baseline parkinsonian motor severity, putaminal DAT activity, the longitudinal LED increment, or long-term motor complications. A previous study reported that PD patients stratified by olfactory tertile had similar baseline UPDRS motor scores and changes in UPDRS scores [6]. The absence of an effect of levodopa use on olfactory performance is additional indirect evidence of no relationship between dopamine and olfaction [35]. Studies using DAT imaging showed no association between putaminal DAT activity and olfactory function [11]. Two studies have reported contradictory results, suggesting that olfactory dysfunction is correlated with higher motor severity and LED, freezing of gait, and putaminal DAT binding [7,36]. However, these studies enrolled PD patients with a wide range of disease durations and did not adjust for the disease duration, which was closely related to motor severity. It would be difficult to investigate the independent relationship between olfactory function and motor function without controlling for this factor. These results suggest that PD patients have similar nigral pathologic burdens regardless of olfactory dysfunction. In terms of motor complications such as WO and LID, low putaminal DAT activity [37], disease severity [38], and a high dose of levodopa39 are risk factors for WO and LID, none of which were associated with baseline olfactory dysfunction in this study. Fullard et al. [6] also found that olfactory dysfunction was not associated with putaminal DAT activity, UPDRS motor score, or disease progression. Therefore, we can infer that early and severe olfactory dysfunction and possible extranigral pathology are unlikely to be associated with presynaptic nigrostriatal degeneration and long-term synaptic plasticity [40].
- This study has several limitations. First, we evaluated olfactory function only based on the aspect of identification, which is thought to require cognitive memory processing [41], even though olfaction can be assessed using various methods, including odor discrimination and detection threshold tasks. Second, we did not monitor UPDRS motor scores regularly, and we did not perform regular neuropsychological tests. Instead, we calculated the LED increment, which has not been validated as a marker reflective of motor progression and monitored the occurrence of motor and cognitive complications. Investigating the association between olfactory dysfunction and the progression of motor and cognitive function is important for the elucidation of the role of olfactory impairment and the pathological spread of nigral and extranigral pathologies in PD. Third, we did not confirm the associations between the nigral and extranigral burden of PD pathology and olfactory dysfunction. Although we used cortical Lewy body involvement to propose a relationship between olfactory and cognitive dysfunction, other possible mechanisms, such as cholinergic dysfunction or concomitant Alzheimer’s disease pathology, could also be associated. Future studies are necessary to investigate these factors to identify the role of olfaction in cognitive decline in PD. Last, this is a retrospective cohort study, which has some disadvantages; the lack of uniformity in baseline evaluations and differential losses to follow-up in some patients may have introduced bias, and the collection of data at different intervals prevented us from identifying an exposed cohort and comparison group appropriately. A prospective study is necessary to clearly identify whether olfactory deficits are an independent risk factor for cognitive complications. Despite these limitations, in this study, we used a large sample of PD patients and investigated motor and cognitive dysfunction in the aspects of baseline function, long-term outcomes, and DAT activity in the same cohort. This resulted in reliable and generalizable results with statistical consistency.
- We demonstrated that baseline olfactory dysfunction was not associated with motor deficits and complications, but it was associated with cognitive dysfunction and dementia conversion. This suggests that early and severe olfactory impairment is likely to be associated with early cortical involvement, probably in the frontotemporal region, and the rapid spreading of Lewy body pathology. Olfactory dysfunction can be a useful biomarker when assessing patients with PD who are at risk of early development of cognitive dysfunction and dementia.
DISCUSSION
Supplementary Materials
Supplementary Table 1
-
Conflicts of Interest
The authors have no financial conflicts of interest.
-
Ethical Standard
All procedures involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards.
-
Author Contributions
Conceptualization: Han Soo Yoo and Phil Hyu Lee. Data curation: Han Soo Yoo and Phil Hyu Lee. Formal analysis: Han Soo Yoo and Seok Jong Chung. Funding acquisition: Phil Hyu Lee. Investigation: Han Soo Yoo, Seok Jong Chung, and Phil Hyu Lee. Methodology: Han Soo Yoo, Seok Jong Chung, and Byoung Seok Ye. Project administration: Young H. Sohn and Phil Hyu Lee. Supervision: Byoung Seok Ye, Young H. Sohn, and Phil Hyu Lee. Visualization: Han Soo Yoo and Seok Jong Chung. Writing—original draft: Han Soo Yoo, Seok Jong Chung, and Phil Hyu Lee. Writing—review & editing: all authors.
Notes
- The authors are grateful to Jungsu S. Oh and Jae Seung Kim (Department of Nuclear Medicine, Asan Medical Center, University of Ulsan College of Medicine) for the quantitative analyses of the 18F-FP-CIT PET images.
- This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (grant number: NRF-2016R1A2A2A05920131).
Acknowledgments
| Variables | Normosmic PD | Hyposmic PD | Anosmic PD | p value |
|---|---|---|---|---|
| Number (%) | 44 (19.3) | 136 (59.6) | 48 (21.1) | < 0.001 |
| Age at onset, y | 62.7 ± 8.4 | 64.9 ± 7.8 | 69.7 ± 6.8 | 0.067*† |
| Male, n (%) | 19 (43.2) | 53 (39.0) | 32 (66.7) | 0.004*† |
| PD onset to CCSIT evaluation, y | 1.3 ± 1.3 | 1.5 ± 1.4 | 1.6 ± 1.5 | 0.530 |
| Follow-up duration, y | 5.9 ± 1.7 | 5.9 ± 1.8 | 5.8 ± 1.9 | 0.890 |
| Total disease duration, y | 7.3 ± 1.8 | 7.4 ± 2.1 | 7.3 ± 2.3 | 0.913 |
| RBD, n (%) | 11 (25.0) | 57 (41.7) | 17 (35.4) | 0.125 |
Data are expressed as the mean ± standard deviation or number (percentage).
* significant difference in the comparison between the normosmic and anosmic PD groups,
† significant difference in the comparison between the hyposmic and anosmic PD groups.
CCSIT: Cross-Cultural Smell Identification Test, PD: Parkinson’s disease, RBD: rapid eye movement sleep behavioral disorder.
| Variables | Normosmic PD | Hyposmic PD | Anosmic PD | p value |
|---|---|---|---|---|
| Motor profile | ||||
| UPDRS motor score | 20.7 (1.46) | 22.85 (0.82) | 24.06 (1.42) | 0.253 |
| Clinical subtype, n (%) | 0.637 | |||
| Tremor dominant | 7 (15.9) | 14 (10.3) | 4 (8.3) | |
| Akineto-rigid | 19 (43.2) | 51 (27.5) | 20 (41.7) | |
| Mixed | 18 (40.9) | 71 (52.2) | 24 (50.0) | |
| DAT activity in posterior putamen | 1.33 (0.08) | 1.41 (0.04) | 1.37 (0.08) | 0.634 |
| Cognitive profile | ||||
| Cognitive status, n (%) | ||||
| Intact cognition/MCI | 35 (79.5)/9 (20.5) | 93 (68.4)/43 (31.6) | 26 (54.2)/22 (45.8) | 0.033* |
| Amnestic/nonamnestic | 6 (66.7)/3 (33.3) | 29 (67.4)/14 (32.6) | 16 (72.7)/6 (27.3) | 0.898 |
| Neuropsychological performance | ||||
| Digit span forward | 0.17 (0.15) | 0.41 (0.09) | 0.19 (0.15) | 0.231 |
| Digit span backward | -0.32 (0.16) | -0.15 (0.09) | -0.23 (0.16) | 0.645 |
| K-BNT | -0.02 (0.15) | -0.23 (0.09) | -0.72 (0.15) | 0.005*† |
| RCFT copy | -0.10 (0.11) | -0.32 (0.19) | -0.52 (0.19) | 0.088 |
| SVLT immediate recall | -0.03 (0.16) | -0.17 (0.09) | -0.44 (0.15) | 0.169 |
| SVLT delayed recall | -0.34 (0.16) | -0.44 (0.09) | -0.52 (0.16) | 0.734 |
| SVLT recognition | 0.08 (0.15) | -0.09 (0.08) | -0.40 (0.15) | 0.079 |
| RCFT immediate recall | -0.36 (0.16) | -0.16 (0.09) | -0.53 (0.16) | 0.106 |
| RCFT delayed recall | -0.19 (0.16) | -0.14 (0.09) | -0.43 (0.15) | 0.260 |
| RCFT recognition | -0.06 (0.16) | -0.03 (0.09) | -0.25 (0.15) | 0.301 |
| COWAT semantic | -0.08 (0.13) | -0.23 (0.07) | -0.36 (0.13) | 0.337 |
| COWAT phonemic | -0.33 (0.17) | -0.13 (0.10) | -0.51 (0.17) | 0.140 |
| Stroop color reading | -0.12 (0.18) | -0.17 (0.10) | -0.73 (0.18) | 0.023*† |
| Total K-MMSE score | 27.33 (0.33) | 27.18 (0.19) | 26.72 (0.32) | 0.397 |
| CDR-SOB | 0.75 (0.11) | 0.82 (0.06) | 1.04 (0.11) | 0.167 |
Data are expressed as an estimated mean (standard error) or number (percentage).
* significant difference in the comparison between the normosmic and anosmic PD groups,
† significant difference in the comparison between the hyposmic and anosmic PD groups.
COWAT: Controlled Oral Word Association Test, CDR-SOB: Clinical Dementia Rating Sum of Boxes, DAT: dopamine transporter, K-BNT: Korean version of the Boston Naming Test, K-MMSE: Korean version of the Mini-Mental State Examination, MCI: mild cognitive impairment, PD: Parkinson’s disease, RCFT: Rey-Osterrieth Complex Figure Test, SVLT: Seoul Verbal Learning Test, UPDRS: Unified Parkinson’s Disease Rating Scale.
|
Univariate |
Multivariate* |
Multivariate† |
||||
|---|---|---|---|---|---|---|
| HR (95% CI) | p value | HR (95% CI) | p value | HR (95% CI) | p value | |
| Group according to CCSIT score | ||||||
| Normosmic group | Reference | Reference | Reference | |||
| Hyposmic group | 1.96 (0.58–6.70) | 0.282 | 1.77 (0.51–6.08) | 0.366 | 1.61 (0.46–5.61) | 0.455 |
| Anosmic group | 5.79 (1.69–19.90) | 0.005 | 3.89 (1.06–14.21) | 0.040 | 3.99 (1.08–14.72) | 0.038 |
| CCSIT as continuous variable | 0.71 (0.61–0.83) | < 0.001 | 0.73 (0.61–0.86) | < 0.001 | 0.73 (0.61–0.87) | < 0.001 |
* adjusted for age, sex, and interval between PD onset and CCSIT evaluation,
† adjusted for age, sex, interval between PD onset and CCSIT evaluation, total Unified Parkinson’s Disease Rating Scale-III score, and cognitive status.
CCSIT: Cross-Cultural Smell Identification Test, CI: confidence interval, HR: hazard ratio, PD: Parkinson’s desease.
- 1. Pellicano C, Benincasa D, Pisani V, Buttarelli FR, Giovannelli M, Pontieri FE. Prodromal non-motor symptoms of Parkinson’s disease. Neuropsychiatr Dis Treat 2007;3:145–152.ArticlePubMedPMC
- 2. Ross GW, Petrovitch H, Abbott RD, Tanner CM, Popper J, Masaki K, et al. Association of olfactory dysfunction with risk for future Parkinson’s disease. Ann Neurol 2008;63:167–173.ArticlePubMed
- 3. Domellöf ME, Lundin KF, Edström M, Forsgren L. Olfactory dysfunction and dementia in newly diagnosed patients with Parkinson’s disease. Parkinsonism Relat Disord 2017;38:41–47.ArticlePubMed
- 4. Braak H, Del Tredici K, Rüb U, de Vos RA, Jansen Steur EN, Braak E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 2003;24:197–211.ArticlePubMed
- 5. Postuma RB, Iranzo A, Hu M, Högl B, Boeve BF, Manni R, et al. Risk and predictors of dementia and parkinsonism in idiopathic REM sleep behaviour disorder: a multicentre study. Brain 2019;142:744–759.ArticlePubMedPMCPDF
- 6. Fullard ME, Tran B, Xie SX, Toledo JB, Scordia C, Linder C, et al. Olfactory impairment predicts cognitive decline in early Parkinson’s disease. Parkinsonism Relat Disord 2016;25:45–51.ArticlePubMedPMC
- 7. Berendse HW, Roos DS, Raijmakers P, Doty RL. Motor and non-motor correlates of olfactory dysfunction in Parkinson’s disease. J Neurol Sci 2011;310:21–24.ArticlePubMed
- 8. Baba T, Kikuchi A, Hirayama K, Nishio Y, Hosokai Y, Kanno S, et al. Severe olfactory dysfunction is a prodromal symptom of dementia associated with Parkinson’s disease: a 3 year longitudinal study. Brain 2012;135:161–169.ArticlePubMedPDF
- 9. Park JW, Kwon DY, Choi JH, Park MH, Yoon HK. Olfactory dysfunctions in drug-naïve Parkinson’s disease with mild cognitive impairment. Parkinsonism Relat Disord 2018;46:69–73.ArticlePubMed
- 10. Camargo CHF, Jobbins VA, Serpa RA, Berbetz FA, Sabatini JS, Teive HAG. Association between olfactory loss and cognitive deficits in Parkinson’s disease. Clin Neurol Neurosurg 2018;173:120–123.ArticlePubMed
- 11. Oh YS, Kim JS, Hwang EJ, Lyoo CH. Striatal dopamine uptake and olfactory dysfunction in patients with early Parkinson’s disease. Parkinsonism Relat Disord 2018;56:47–51.ArticlePubMed
- 12. Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 2010;25:2649–2653.ArticlePubMed
- 13. Doty RL, Marcus A, Lee WW. Development of the 12-item Cross-Cultural Smell Identification Test (CC-SIT). Laryngoscope 1996;106:353–356.ArticlePubMed
- 14. Lee JE, Cho KH, Ham JH, Song SK, Sohn YH, Lee PH. Olfactory performance acts as a cognitive reserve in non-demented patients with Parkinson’s disease. Parkinsonism Relat Disord 2014;20:186–191.ArticlePubMed
- 15. Oh M, Kim JS, Kim JY, Shin KH, Park SH, Kim HO, et al. Subregional patterns of preferential striatal dopamine transporter loss differ in Parkinson disease, progressive supranuclear palsy, and multiple-system atrophy. J Nucl Med 2012;53:399–406.ArticlePubMed
- 16. Jin S, Oh M, Oh SJ, Oh JS, Lee SJ, Chung SJ, et al. Differential diagnosis of parkinsonism using Dual-phase F-18 FP-CIT PET imaging. Nucl Med Mol Imaging 2013;47:44–51.ArticlePubMedPDF
- 17. Eggers C, Kahraman D, Fink GR, Schmidt M, Timmermann L. Akineticrigid and tremor-dominant Parkinson’s disease patients show different patterns of FP-CIT single photon emission computed tomography. Mov Disord 2011;26:416–423.ArticlePubMed
- 18. Ahn HJ, Chin J, Park A, Lee BH, Suh MK, Seo SW, et al. Seoul Neuropsychological Screening Battery-Dementia version (SNSB-D): a useful tool for assessing and monitoring cognitive impairments in dementia patients. J Korean Med Sci 2010;25:1071–1076.ArticlePubMedPMC
- 19. Cecchini MP, Federico A, Zanini A, Mantovani E, Masala C, Tinazzi M, et al. Olfaction and taste in Parkinson’s disease: the association with mild cognitive impairment and the single cognitive domain dysfunction. J Neural Transm 2019;126:585–595.ArticlePubMedPDF
- 20. Yoo HS, Jeon S, Chung SJ, Yun M, Lee PH, Sohn YH, et al. Olfactory dysfunction in Alzheimer’s disease- and Lewy body-related cognitive impairment. Alzheimers Dement 2018;14:1243–1252.ArticlePubMed
- 21. Hawkes CH, Del Tredici K, Braak H. Parkinson’s disease: a dual-hit hypothesis. Neuropathol Appl Neurobiol 2007;33:599–614.ArticlePubMedPMC
- 22. Baba T, Takeda A, Kikuchi A, Nishio Y, Hosokai Y, Hirayama K, et al. Association of olfactory dysfunction and brain. Metabolism in Parkinson’s disease. Mov Disord 2011;26:621–628.ArticlePubMed
- 23. Bohnen NI, Müller MLTM, Kotagal V, Koeppe RA, Kilbourn MA, Albin RL, et al. Olfactory dysfunction, central cholinergic integrity and cognitive impairment in Parkinson’s disease. Brain 2010;133:1747–1754.ArticlePubMedPMCPDF
- 24. Morley JF, Weintraub D, Mamikonyan E, Moberg PJ, Siderowf AD, Duda JE. Olfactory dysfunction is associated with neuropsychiatric manifestations in Parkinson’s disease. Mov Disord 2011;26:2051–2057.ArticlePubMedPMC
- 25. Lee EY, Eslinger PJ, Du G, Kong L, Lewis MM, Huang X. Olfactory-related cortical atrophy is associated with olfactory dysfunction in Parkinson’s disease. Mov Disord 2014;29:1205–1208.ArticlePubMedPMC
- 26. Damasio H, Grabowski TJ, Tranel D, Ponto LLB, Hichwa RD, Damasio AR. Neural correlates of naming actions and of naming spatial relations. Neuroimage 2001;13:1053–1064.ArticlePubMed
- 27. Yun JY, Lee DY, Seo EH, Choo IH, Park SY, Kim SG, et al. Neural correlates of stroop performance in Alzheimer’s disease: a FDG-PET study. Dement Geriatr Cogn Dis Extra 2011;1:190–201.ArticlePubMedPMC
- 28. Dintica CS, Marseglia A, Rizzuto D, Wang R, Seubert J, Arfanakis K, et al. Impaired olfaction is associated with cognitive decline and neurodegeneration in the brain. Neurology 2019;92:e700–e709.ArticlePubMedPMC
- 29. Roberts RO, Christianson TJH, Kremers WK, Mielke MM, Machulda MM, Vassilaki M, et al. Association between olfactory dysfunction and amnestic mild cognitive impairment and Alzheimer disease dementia. JAMA Neurol 2016;73:93–101.ArticlePubMedPMC
- 30. Arendt T, Bigl V, Arendt A, Tennstedt A. Loss of neurons in the nucleus basalis of Meynert in Alzheimer’s disease, paralysis agitans and Korsakoff’s disease. Acta Neuropathol 1983;61:101–108.ArticlePubMedPDF
- 31. Shimada H, Hirano S, Shinotoh H, Aotsuka A, Sato K, Tanaka N, et al. Mapping of brain acetylcholinesterase alterations in Lewy body disease by PET. Neurology 2009;73:273–278.ArticlePubMed
- 32. Tsuboi Y, Wszolek ZK, Graff-Radford NR, Cookson N, Dickson DW. Tau pathology in the olfactory bulb correlates with Braak stage, Lewy body pathology and apolipoprotein ɛ4. Neuropathol Appl Neurobiol 2003;29:503–510.ArticlePubMed
- 33. Dintica CS, Marseglia A, Rizzuto D, Wang R, Seubert J, Arfanakis K, et al. Impaired olfaction is associated with cognitive decline and neurodegeneration in the brain. Neurology 2019;92:e700–e709.ArticlePubMedPMC
- 34. Irwin DJ, Grossman M, Weintraub D, Hurtig HI, Duda JE, Xie SX, et al. Neuropathological and genetic correlates of survival and dementia onset in synucleinopathies: a retrospective analysis. Lancet Neurol 2017;16:55–65.ArticlePubMedPMC
- 35. Doty RL, Stern MB, Pfeiffer C, Gollomp SM, Hurtig HI. Bilateral olfactory dysfunction in early stage treated and untreated idiopathic Parkinson’s disease. J Neurol Neurosurg Psychiatry 1992;55:138–142.ArticlePubMedPMC
- 36. Cavaco S, Goncalves A, Mendes A, Vila-Chã N, Moreira I, Fernandes J, et al. Abnormal olfaction in Parkinson’s disease is related to faster disease progression. Behav Neurol 2015;2015:976589.ArticlePubMedPMCPDF
- 37. Chung SJ, Lee Y, Oh JS, Kim JS, Lee PH, Sohn YH. Putaminal dopamine depletion in de novo Parkinson’s disease predicts future development of wearing-off. Parkinsonism Relat Disord 2018;53:96–100.ArticlePubMed
- 38. Parkinson Study Group. Impact of deprenyl and tocopherol treatment on Parkinson’s disease in DATATOP patients requiring levodopa. Ann Neurol 1996;39:37–45.ArticlePubMed
- 39. Hauser RA, McDermott MP, Messing S. Factors associated with the development of motor fluctuations and dyskinesias in Parkinson disease. Arch Neurol 2006;63:1756–1760.ArticlePubMed
- 40. Ahlskog JE, Muenter MD. Frequency of levodopa-related dyskinesias and motor fluctuations as estimated from the cumulative literature. Mov Disord 2001;16:448–458.ArticlePubMed
- 41. Hedner M, Larsson M, Arnold N, Zucco GM, Hummel T. Cognitive factors in odor detection, odor discrimination, and odor identification tasks. J Clin Exp Neuropsychol 2010;32:1062–1067.ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Correlation of olfactory function factors with cardiac sympathetic denervation in Parkinson’s disease
Dong-Woo Ryu, Sang-Won Yoo, Ko-Eun Choi, Yoon-Sang Oh, Joong-Seok Kim
Journal of Neurology.2024; 271(3): 1397. CrossRef - Estimating motor progression trajectory pursuant to temporal dynamic status of cardiac denervation in Parkinson’s disease
Sang-Won Yoo, Dong-Woo Ryu, Yoon-Sang Oh, Seunggyun Ha, Chul Hyoung Lyoo, Yuna Kim, Ji-Yeon Yoo, Joong-Seok Kim
Journal of Neurology.2024; 271(4): 2019. CrossRef - Olfactory Dysfunction in Parkinson’s Disease, Its Functional and Neuroanatomical Correlates
Gabriel Torres-Pasillas, Donají Chi-Castañeda, Porfirio Carrillo-Castilla, Gerardo Marín, María Elena Hernández-Aguilar, Gonzalo Emiliano Aranda-Abreu, Jorge Manzo, Luis I. García
NeuroSci.2023; 4(2): 134. CrossRef - Impact of deep brain stimulation (DBS) on olfaction in Parkinson's disease: Clinical features and functional hypotheses
G. Brand, C. Bontempi, L. Jacquot
Revue Neurologique.2023; 179(9): 947. CrossRef - Sequential change in olfaction and (non) motor symptoms: the difference between anosmia and non-anosmia in Parkinson’s disease
Ting-Chun Fang, Yu-Shan Tsai, Ming-Hong Chang
Frontiers in Aging Neuroscience.2023;[Epub] CrossRef - Traumatic brain injury-induced inflammatory changes in the olfactory bulb disrupt neuronal networks leading to olfactory dysfunction
Xiang Liu, Zhuofan Lei, Dylan Gilhooly, Junyun He, Yun Li, Rodney M. Ritzel, Hui Li, Long-Jun Wu, Shaolin Liu, Junfang Wu
Brain, Behavior, and Immunity.2023; 114: 22. CrossRef - Serum Biomarkers of Olfactory Identification Deficits in Patients with Parkinson’s Disease
Fu-Jia Li, Yang-Dan-Yu Li, Xu Liu, Jie Zu, Wei Zhang, Qi-Hua Xiao, Xue-Bin Niu, Li Du, Chen-Chen Cui, Ru-Yu Zhang, Xiao-Qing He, Gui-Yun Cui, Chuan-Ying Xu, Dominic B. Fee
Acta Neurologica Scandinavica.2023; 2023: 1. CrossRef - UPSIT subitems may predict motor progression in Parkinson’s disease
Yu-Hsuan Lin, Ting-Chun Fang, Hsin-Bei Lei, Shih-Chi Chiu, Ming-Hong Chang, Yi-Jen Guo
Frontiers in Neurology.2023;[Epub] CrossRef - Olfactory dysfunction is associated with motor function only in tremor-dominant Parkinson’s disease
Fardin Nabizadeh, Kasra Pirahesh, Elham Khalili
Neurological Sciences.2022; 43(7): 4193. CrossRef - Novel diagnostic tools for identifying cognitive impairment using olfactory-stimulated functional near-infrared spectroscopy: patient-level, single-group, diagnostic trial
Jaewon Kim, Dong Keon Yon, Kyu Yeong Choi, Jang Jae Lee, Namwoo Kim, Kun Ho Lee, Jae Gwan Kim
Alzheimer's Research & Therapy.2022;[Epub] CrossRef - The Role of Olfactory System in the Etiogenesis of Parkinson’s Diseases: An Overview
Jiju Narayanan Avanipully, Dithu Thekkekkara, Sahyadri M, Vipan K. Parihar, Santhepete Nanjundaiah Manjula
Journal of Pharmacology and Pharmacotherapeutics.2022; 13(1): 31. CrossRef - International consensus statement on allergy and rhinology: Olfaction
Zara M. Patel, Eric H. Holbrook, Justin H. Turner, Nithin D. Adappa, Mark W. Albers, Aytug Altundag, Simone Appenzeller, Richard M. Costanzo, Ilona Croy, Greg E. Davis, Puya Dehgani‐Mobaraki, Richard L. Doty, Valerie B. Duffy, Bradley J. Goldstein, David
International Forum of Allergy & Rhinology.2022; 12(4): 327. CrossRef - Does Olfactory Dysfunction Correlate with Disease Progression in Parkinson’s Disease? A Systematic Review of the Current Literature
Tommaso Ercoli, Carla Masala, Gianluca Cadeddu, Marcello Mario Mascia, Gianni Orofino, Angelo Fabio Gigante, Paolo Solla, Giovanni Defazio, Lorenzo Rocchi
Brain Sciences.2022; 12(5): 513. CrossRef - Olfactory dysfunction and striatal dopamine transporter binding in motor subtypes of Parkinson’s disease
Fardin Nabizadeh, Fatemeh Sodeifian, Kasra Pirahesh
Neurological Sciences.2022; 43(8): 4745. CrossRef - Olfaction and Executive Cognitive Performance: A Systematic Review
Vasudeva Murthy Challakere Ramaswamy, Peter William Schofield
Frontiers in Psychology.2022;[Epub] CrossRef - Nasal and Parotid Blood Pool Activity Is Significantly Correlated with Metabolic Syndrome Components and Sleep Apnea
William T. Phillips, Nasser J. Issa, Shereef B. Elhalwagi, Hilda T. Draeger, Joyce G. Schwartz, Jonathan A. Gelfond
Metabolic Syndrome and Related Disorders.2022; 20(7): 395. CrossRef - Chronic neuropsychiatric sequelae of SARS‐CoV‐2: Protocol and methods from the Alzheimer's Association Global Consortium
Gabriel A. de Erausquin, Heather Snyder, Traolach S. Brugha, Sudha Seshadri, Maria Carrillo, Rajesh Sagar, Yueqin Huang, Charles Newton, Carmela Tartaglia, Charlotte Teunissen, Krister Håkanson, Rufus Akinyemi, Kameshwar Prasad, Giovanni D'Avossa, Gabriel
Alzheimer's & Dementia: Translational Research & Clinical Interventions.2022;[Epub] CrossRef - Machine learning-based prediction of cognitive outcomes in de novo Parkinson’s disease
Joshua Harvey, Rick A. Reijnders, Rachel Cavill, Annelien Duits, Sebastian Köhler, Lars Eijssen, Bart P. F. Rutten, Gemma Shireby, Ali Torkamani, Byron Creese, Albert F. G. Leentjens, Katie Lunnon, Ehsan Pishva
npj Parkinson's Disease.2022;[Epub] CrossRef - Impact of Subthalamic Deep Brain Stimulation on Hyposmia in Patients With Parkinson's Disease Is Influenced by Constipation and Dysbiosis of Microbiota
Chao Li, Ying Hou, Xu Wang, Yue-xuan Li, Feng Li, Chao Zhang, Wei-guo Li
Frontiers in Neurology.2021;[Epub] CrossRef - Hyposmia may predict development of freezing of gait in Parkinson’s disease
Jae Jung Lee, Jin Yong Hong, Jong Sam Baik
Journal of Neural Transmission.2021; 128(6): 763. CrossRef - Clinical and Dopamine Depletion Patterns in Hyposmia- and Dysautonomia-Dominant Parkinson’s Disease
Han Soo Yoo, Sangwon Lee, Seong Ho Jeong, Byoung Seok Ye, Young H. Sohn, Mijin Yun, Phil Hyu Lee
Journal of Parkinson's Disease.2021; 11(4): 1703. CrossRef
Comments on this article
- Figure
- Related articles
-
- Investigation of the Long-Term Effects of Amantadine Use in Parkinson’s Disease
- Potential Link Between Cognition and Motor Reserve in Patients With Parkinson’s Disease
- Association Between Gait and Dysautonomia in Patients With De Novo Parkinson’s Disease: Forward Gait Versus Backward Gait
- Umami and Other Taste Perceptions in Patients With Parkinson’s Disease
- The Supplementary Motor Complex in Parkinson’s Disease
 KMDS
KMDS
 E-submission
E-submission
 PubReader
PubReader ePub Link
ePub Link Cite
Cite