Knowledge, Attitude, and Perceptions about Deep Brain Stimulation for Parkinson’s Disease: Observations from a Single Indian Center
Article information
Abstract
Objective
Willingness to undergo deep brain stimulation (DBS) among patients with Parkinson’s disease (PD) and their overall satisfaction with the procedure is highly dependent upon expectations, which are based on the core concepts of knowledge, attitude and perceptions. The present study aims to evaluate these factors in patients and caregivers with PD from a single tertiary care hospital in India.
Methods
A structured questionnaire designed to assess the knowledge, attitude and perceptions about DBS in PD was administered to 400 patients with PD and their caregivers.
Results
A very small proportion of patients and caregivers were aware of DBS. Even those who claimed to be aware of DBS were inadequately informed and had incorrect knowledge, which led to wrong attitudes and perceptions.
Conclusion
There are very significant knowledge gaps and misconceptions regarding DBS among patients with PD and caregivers. Adequate and appropriate education is necessary to clarify these misconceptions to avoid the development of unrealistic expectations and poor satisfaction.
Deep brain stimulation (DBS) has been well established as a treatment modality in patients with advanced Parkinson’s disease (PD) with motor fluctuations [1]. However, willingness to undergo DBS and overall satisfaction is a product of knowledge, attitudes and perceptions about DBS. Knowledge is the capacity to acquire, retain and use information appropriately; attitudes are the inclination to react to a situation; and perceptions are thoughts, beliefs or opinions about a subject [2]. These variables are interlinked and lead to expectations and eventual satisfaction or dissatisfaction. A thorough understanding of these factors is crucial to prevent postoperative disappointment.
Education, sociocultural background, economic status, caregiver support and the structure of the healthcare system play a significant role in determining knowledge and attitudes. Several studies have explored these aspects in patients with PD [3-18], but to the best of our knowledge, there are no such studies from India. Geographical location is paramount since it definitely influences the above factors. Previous studies have primarily focused on patients with PD who have undergone DBS. Caregivers who play a significant role in patient care and the decision-making process regarding DBS have rarely been evaluated. The present study aims to evaluate the knowledge about, attitudes toward, and perceptions of DBS in patients with PD and caregivers from a single tertiary care hospital in India.
MATERIALS & METHODS
Subject recruitment and assessment
Consecutive patients diagnosed with PD and the caregivers who accompanied them were recruited from the neurology outpatient department and movement disorder clinic over a period of 10 months. Those who visited alone, were already counselled about the need for DBS, or had undergone DBS were excluded from the study. Participants responding “Yes” to the question “Are you aware of DBS for PD?” were administered a structured questionnaire comprising open-ended questions designed to assess their knowledge about, attitudes toward and perceptions of DBS (Supplementary Table 1 in the online-only Data Supplement). Basic demographic data such as age, gender, education, and socioeconomic status (SES) were collected from both patients and caregivers. The clinical data included age at onset (AAO), duration of illness, Hoehn and Yahr (H&Y) stage, Unified Parkinson’s Disease Rating Scale-III (UPDRS-III), levodopa equivalent daily dose (LEDD), and the presence or absence of dyskinesia. This study was approved by the institute ethics committee (NO. NIMH/DO/IEC (BS&NS DIV)/2017-18).
Statistical evaluation
The awareness of DBS was evaluated for dyads, i.e., patient and caregiver responses were considered together and separately at the patient and caregiver levels. Subgroup analysis was performed between patients who were aware and unaware of DBS and for caregivers who were aware and unaware of DBS. Logistic regression analysis was performed to evaluate the role of demographic and clinical variables in predicting awareness of DBS. Student’s t test was used for continuous variables, and the chi-square test was used for categorical variables. The level of significance was set at p < 0.05.
RESULTS
The majority of caregivers in this study were spouses (49.25%, n = 197), followed by their children (47%, n = 188), siblings (3%, n = 12), and friends (0.75%, n = 3). At least one member of the dyad, i.e., patient or caregiver, or both, was aware of DBS in 102 dyads (Supplementary Figure 1 in the online-only Data Supplement). Only 18.00% (n = 72) of patients responded “Yes” to the question “Are you aware of DBS for PD?,” while 20.25% (n = 81) of caregivers reported being aware of DBS.
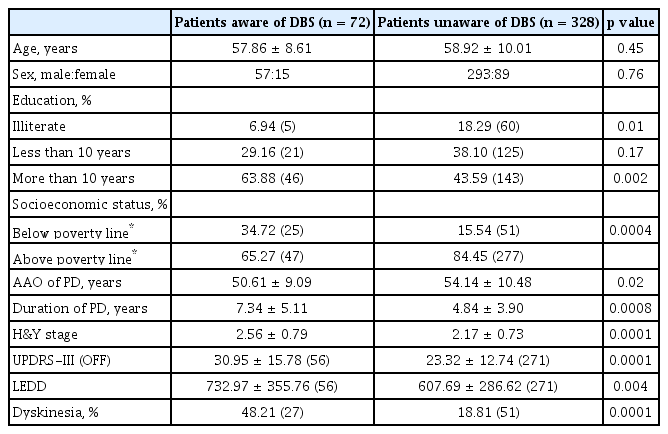
In comparison to patients who were unaware of DBS, those who were aware of DBS had a significantly higher level of education, better SES, younger AAO, longer duration of illness, a higher H&Y stage, a higher UPDRS-III OFF score, a higher LEDD, and a higher prevalence of dyskinesia (Table 1). Logistic regression analysis revealed that in addition to disease severity, educational status (p = 0.001) and SES (p = 0.019) were also predictors of knowledge about DBS. Patients with a higher educational status had higher odds of knowing about DBS, and those with a lower SES had lower odds of knowing about DBS. Doctors were the primary source of information, and the majority of patients learned about DBS within five years of illness (4.82 ± 4.08 years) (Table 2). The average cost of DBS reported by patients was 1,215,000 ± 1,050,000 INR (16,000 ± 13,800 USD). “Electrodes are implanted in the brain and stimulated from a battery” was the most common response to how DBS works. Only 26.83% (n = 19) were aware of the types of DBS batteries, and a few respondents assumed that DBS could cure PD. Most patients who were aware of DBS were undecided about wanting to undergo DBS at the time of interview (62.50%, n = 45), and of those wishing to defer DBS (13.88%, n = 10), the inability to afford the surgery (30%, n = 3) and apprehension (30%, n = 30) were the most common reasons.
Caregivers who were aware of DBS predominantly were mostly children of patients and were well educated. Most responses provided by caregivers who were aware of DBS were comparable to those provided by patients who were aware of DBS (Table 2). In comparison to patients, caregivers had more vague answers pertaining to how DBS works: the majority of caregivers were unaware of the types of batteries, and a small proportion of them thought that DBS could cure PD. Although the difference was not significant, fewer caregivers than patients knew about the need to continue medications, and a higher percentage of caregivers knew that life-long programming was necessary. Similar to patients, most caregivers who wanted to defer DBS reported that financial constraints were the deciding factor.
DISCUSSION
We observed that a very small proportion of patients and caregivers were aware of DBS. Even those who claimed awareness about DBS were inadequately informed with incorrect knowledge, which led to misperceptions. The assessment of caregiver knowledge is critical, for as evidenced by our results, most caregivers were either unaware of DBS, or even if they were aware, they harbored several misconceptions. These misconceptions, if left unclarified, will lead to unrealistic expectations for DBS and may be highly detrimental, as long-term care for a patient undergoing DBS needs definite solidarity and an involved caregiver [5]. Furthermore, in India, the caregiver is typically a family member, and the availability of and access to long-term care facilities with nursing support is limited. These observations are important, as they shed light on the basis for patient and caregiver expectations and outcomes after DBS.
Our patients had a significantly lower awareness of DBS than patients in previous reports (24.3% to 91.3%) [10,11,18] but had a markedly higher awareness than the 5.5% of the general population in South Korea who were aware of surgical treatment for PD [19]. Caregiver awareness has not been previously reported. The main factors that influenced awareness of DBS were education, SES, and severity of illness. Patients who had a higher educational and SES, higher disease severity based on H&Y stage, UPDRS-III scores, and dyskinesias were more likely to be aware of DBS. Patients who had a more advanced illness with an inadequate response to medication were more likely to voluntarily attempt to explore other options of treatment. Education also appears to play a critical role, and illiterate participants in our cohort were more likely to be unaware of DBS. Based on the 2011 census in India, approximately 73.5% of the literate Indian population has less than 10 years of education. In our cohort, 43.58% of educated patients and 35.29% of educated caregivers had less than 10 years of education. Neurologists were the main source of knowledge in our study and in previous reports from China [18] and North America [20]. In Europe, PD support groups are the main source of information [10,11]. The limited number of DBS education resources available to a less literate population may contribute to the low level of awareness. Educational materials should be tailored to cater to ethnic, cultural and educational backgrounds. For instance, all information, whether audiovisual or print should be made available in the patient’s and caregiver’s language, the material should include minimal medical jargon, and it should include information that dispels common myths about DBS.
Despite being aware of DBS, patient and caregiver responses suggested that the knowledge possessed by these subjects was definitely inadequate and often incorrect. Knowledge pertaining to the cost of surgery and knowing how DBS works has a strong bearing on attitudes, as evidenced by the reasons provided by patients and caregivers to refrain from surgery. The cost of DBS in India ranges from 9,000 USD to 23,000 USD depending upon the type of battery, hospital (government vs. private), etc. Although most patients and caregivers in our study provided correct estimates, a few gave grossly incorrect responses. Financial burden [16], fear of the surgical procedure [20], and possible adverse effects [10,16,20] have been previously reported as factors for reluctance to undergo DBS. Better knowledge, caregivers and economic support were found to allay these fears [16]. In the general population, 88% of individuals were willing to undergo surgical treatment for DBS if indicated [19]. Assumptions that DBS cures PD, assumptions that no medication will be required post-surgery, and a lack of awareness about post-DBS programming also contributes to low levels of postsurgical satisfaction, which has been previously reported [15]. Increased knowledge about DBS as well as caregiver and economic support were found to allay these fears [16].
There are limitations to this study. The caregivers interviewed may not necessarily have been the primary caregivers. Most participants were from a middle to low SES, with low levels of literacy. This cohort forms the majority of our community, and our results may reflect baseline knowledge. However, a nationwide, multicenter study is necessary to validate our findings and discern the actual status of this issue across India. Finally, responses to descriptive questions were not recorded verbatim.
CONCLUSIONS
There are very significant knowledge gaps and misconceptions about DBS in patients with PD and their caregivers. Adequate and timely education and clarification are pertinent to allay the development of apprehensions and prevent the establishment of unrealistic expectations and low levels of postoperative satisfaction.
Supplementary Material
The online-only Data Supplement is available with this article at https://doi.org/10.14802/jmd.20066.
Supplementary Table 1.
Structured questionnaire administered to patients and caregivers who were aware of DBS
Supplementary Figure 1.
A: Percentage of dyads who were aware and unaware of DBS in Parkinson’s disease. B: Percentage of patients who were aware and unaware of DBS. C: Percentage of caregivers who were aware and unaware of DBS. P+C+: patient aware, caregiver aware, P+C-: patient aware, caregiver unaware, P-C+: patient unaware, caregiver aware, DBS: deep brain stimulation.
Notes
Conflicts of Interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Shweta Prasad, Lulup Kumar Sahoo, Dhruv Batra, Nitish Kamble, Pramod Kumar Pal. Data curation: Shweta Prasad, Amitabh Bhattacharya, Lulup Kumar Sahoo, Dhruv Batra. Formal analysis: Shweta Prasad, Amitabh Bhattacharya. Investigation: Shweta Prasad, Amitabh Bhattacharya, Lulup Kumar Sahoo, Dhruv Batra. Methodology: Shweta Prasad, Amitabh Bhattacharya, Lulup Kumar Sahoo, Dhruv Batra, Pramod Kumar Pal. Project administration: Nitish Kamble, Ravi Yadav, Pramod Kumar Pal. Resources: Nitish Kamble, Ravi Yadav, Pramod Kumar Pal. Supervision: Nitish Kamble, Ravi Yadav, Pramod Kumar Pal. Validation: Nitish Kamble, Ravi Yadav, Pramod Kumar Pal. Visualization: Shweta Prasad, Amitabh Bhattacharya. Writing—original draft: Shweta Prasad. Writing—review & editing: all authors. Approval of final manuscript: all authors.
Acknowledgements
None.