Bupropion-Induced Dystonia in a Patient with Parkinson’s Disease
Article information
Acute dystonic reactions are characterized by involuntary contraction of the muscles of the extremities, face, neck, abdomen, pelvis or larynx, in either sustained or intermittent patterns, that lead to abnormal movements or postures [1]. These reactions are common with drugs that block dopamine D2 receptors, causing dopaminergic-cholinergic imbalance in the basal ganglia. These include typical antipsychotics; some atypical antipsychotics, such as risperidone and olanzapine; antidepressants, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs); and some antiepileptic drugs, such as carbamazepine and phenytoin. Bupropion belongs to a group of aminoketones used widely for major depressive disorders, smoking cessation and sexual dysfunction secondary to SSRIs. It is a nonselective inhibitor of dopamine and noradrenaline transport and reduces the uptake of dopamine and noradrenaline [2]. There are cases of dystonia reported after taking bupropion with dosages as small as 75 mg [3]. Here, we report a case of severe dystonic reaction in an elderly female patient with Parkinson’s disease (PD) after taking bupropion.
A 78-year-old woman with PD for 14 years presented with excessive on and off motor symptoms for the previous three years. She also suffered from hypertension and major depressive disorder for 16 years and had a history of suicide attempts for which she was prescribed quetiapine and venlafaxine. The patient had been admitted for the optimization of medications in view of motor fluctuations and was on a combination of levodopa, carbidopa, entacapone and ropinirole. On admission, she had PD, Hoehn and Yahr stage 5, and a Unified Parkinson’s Disease Rating Scale score of 148 (part 1, 23; part 2, 32; part 3, 81; part 4, 12). The “on” symptoms would consist of excessive dyskinesias of both the upper and the lower limbs with orolingual dyskinesias, while the “off” symptoms would consist of excessive rigidity of both the upper and the lower limbs, severe hypophonia and low mood.
On psychiatric evaluation, she had low mood, depression, ideas of suspicion, reference, self-harm and suicidal ideation. She was prescribed venlafaxine and sertraline. However, she developed hyponatremia (118 mg/dL serum sodium). In view of sertraline’s potential to cause hyponatremia, it was discontinued, and oral salt intake was increased, with which the sodium level increased to 125 mg/dL and 136 mg/dL after 3 and 6 days, respectively. Bupropion 150 mg once a day was subsequently administered. After the first dose of bupropion, the patient complained of dry mouth. On the subsequent day after taking bupropion, she started having increased abnormal involuntary movements of both the upper and the lower limbs. These movements were more severely disabling than her regular “on” period dyskinesias. The dyskinesias were followed by severe dystonia in both the upper and the lower limbs. The patient also had trismus, risus sardonicus and dysphagia comprising buccolingual crisis along with left laterocollis. She complained of feeling something persistently stuck to her tongue and abnormal sensations in the tongue pertaining possibly to feeling pseudomacroglosia. She had severe laryngeal dystonia leading to an inability to produce comprehensible speech or swallow.
In a patient with advanced PD with already fluctuating baseline symptoms and severe “on” period symptoms, a suspicion and confirmation of bupropion-induced adverse reaction was difficult. The Naranjo algorithm [4] and Abnormal Involuntary Movement Scale (AIMS) [5] were utilized for patient assessment. The patient had a Naranjo scale score of 7, suggesting a probable bupropion-induced adverse drug reaction (Table 1). Bupropion was discontinued, nasogastric tube feeding for severe dysphagia was instituted, and 50 mg diphenhydramine was administered, followed by 25 mg every 6 hours for 2 days. The AIMS showed scores of 33 on day 1, 22 on day 2 and 13 on day 3, showing improvement after drug discontinuation (Supplementary Table 1 in the online-only Data Supplement). Her symptoms started reducing gradually, with trismus and laterocollis being the first to resolve. Dysphagia, laryngeal dystonia and extremity dystonia lasted for more than 48 hours.
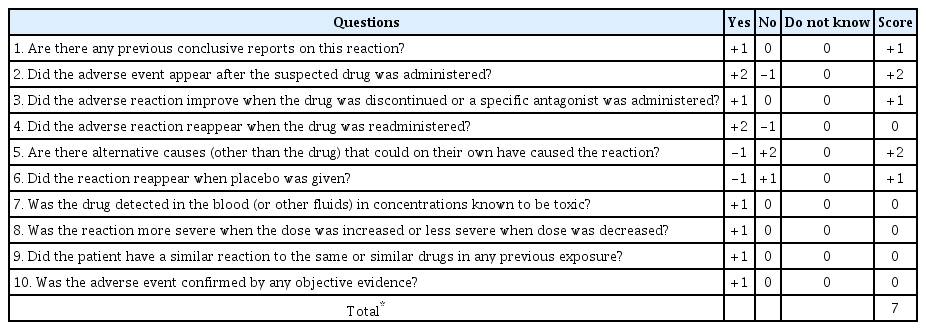
Naranjo algorithm of the patient showing score 7 (probable drug induced dystonic reaction) on day 2 of bupropion administration
The few characteristic drug-related dystonic reactions include buccolingual crisis, oculogyric crisis, torticollic crisis, tortipelvic crisis, opisthotonic crisis, laryngeal dystonia and pseudomacroglosia [1]. This case highlights bupropion-related severe acute dystonic reaction in an elderly woman with PD and major depressive disorder. Our patient developed bilateral upper and lower extremity dystonia, buccolingual crisis, left laterocollis, pseudomacroglossia and severe laryngeal dystonia after only two doses of bupropion.
Bupropion is often preferred in patients with extrapyramidal disorders for the management of depressive symptoms because of its mechanism of increasing dopamine levels. However, there have been few documented cases of acute dystonia after even a single dose of bupropion [3]. Bupropion-induced dystonia was noted in younger males with additional SSRI use, which may have potentiated dystonia due to the stimulatory action of serotonin on central dopaminergic pathways. The predictors of drug-induced dystonia are multifactorial, including younger age, male sex, typical antipsychotic drugs, a high dosage of the inciting drug or concomitant inducers [6].
In the present case, dystonia occurred in an elderly female with PD who was already on dopaminergic drugs and had significant motor and nonmotor on-off symptoms. Unlike dystonia due to SSRIs, bupropion is a dopamine and noradrenaline reuptake inhibitor with no known effect on serotonergic inputs. Pathophysiologically, dystonia developing with bupropion can be considered similar to dopamine-induced peak dose dystonia by its mechanism of increasing the availability of dopamine [4]. Patients with late PD with a high degree of nigral degeneration have disturbances in pre- and postsynaptic nigrostriatal dopamine transmission that lead to plasticity changes postsynaptically and the supersensitivity of postsynaptic dopaminergic neurons [7]. The most sensitive receptors are likely situated in the dorsal putamen, where striatal dopaminergic denervation is greatest. D2 dopamine receptors, which are most abundantly present in the matrix of the striatum, are proposed to be mainly involved, and selective stimulation of these D2 receptors may induce dystonia [7]. Significantly, patients with advanced-stage PD and severe on-off phenomena may become victims of delayed clinical suspicion of adverse drug-induced reactions. The Naranjo algorithm is a questionnaire for determining the likelihood that an adverse drug reaction after taking a drug is actually due to the drug rather than any other factors [4]. This, along with the AIMS, can help assess the progression and regression of drug-induced dyskinetic movements and dystonia in a patient with PD [4,5].
This case emphasizes the need for a cautious approach to the management of depression and the use of dopamine reuptake inhibitors in a patient with underlying extrapyramidal disorders. The development of severe acute dystonic reactions must be kept in mind and carefully assessed while administering bupropion in patients with PD on dopaminergic therapy.
Supplementary Material
The online-only Data Supplement is available with this article at https://doi.org/10.14802/jmd.20046.
Supplementary Table 1.
Abnormal Involuntary Movement Scale (AIMS) in a patient with drug-related dystonia
Notes
Conflicts of Interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Samhita Panda. Data curation: Monalisa Vegda. Formal analysis: Samhita Panda, Monalisa Vegda. Investigation: Monalisa Vegda. Methodology: Samhita Panda. Project administration: Monalisa Vegda. Supervision: Samhita Panda. Validation: Samhita Panda. Visualization: Samhita Panda, Monalisa Vegda. Writing—original draft: Monalisa Vegda. Writing—review & editing: Samhita Panda.
Acknowledgements
None.
