Clinical Characteristics of Involuntary Movement in Hospitalized Patients
Article information
Abstract
Objective
Neurological symptoms in hospitalized patients are not rare, and neurological consultation for movement disorders is especially important in evaluating or managing those with various movement disorders. Therefore, we investigated a clinical pattern of in-hospital consultations for various movement disorders in a tertiary care university hospital.
Methods
Over two years, a total of 202 patients (70.7 ± 11.8 years of age) presenting with movement disorders referred to movement disorder specialists were investigated.
Results
The main symptoms referred by nonneurologists were tremor (56.9%), parkinsonism (16.8%), and gait disturbance (8.9%). The most frequent diagnostic category was toxic/metabolic-caused movement disorder (T/MCMD) (35%) with regard to medications, followed by Parkinson’s disease (PD) (16%). Regarding the mode of onset, T/MCMD was the leading cause for acute (68%) and subacute onset (46%), while PD was the leading disorder (31%) for chronic onset.
Conclusion
The current study showed a characteristic pattern of inpatients presenting with movement disorders. Furthermore, our findings highlighted the clinical significance of drug use or metabolic problems for treating this patient population.
Movement disorders alter the function of the central nervous system. These movement disorders are not related to muscular weakness or spasticity. They are divided into two major categories: hyperkinesia defined as an excess of involuntary movement, and hypokinesia, a decrease or lack of voluntary and/or automatic movement. The majority of movement disorders have a slowly progressive course, implicating a primary neurodegenerative disease. However, a number of movement disorders have a rapid onset that may be linked with the adverse effects of medications or a metabolic condition. To accurately diagnose patients presenting with a movement disorder, it is necessary to perform a thorough neurological examination and history taking. Consequently, there has been a recent increase in clinical awareness of the subspecialty of movement disorders.
Neurological problems are relatively common in hospitalized patients, and a neurological consultation is often critical for the proper evaluation and/or management of those conditions [1,2]. Therefore, nonneurological physicians or surgeons frequently ask about their patient’s neurological symptoms. Movement disorders are a distinct category of neurological disorders that are inherently difficult to diagnose properly. Due to the complexity and distinctiveness of movement disorders, physicians are especially concerned when patients present with involuntary or abnormal movement indicative of a movement disorder. Moreover, inpatients might have particular situations in which movement disorders develop or more serious and complicated medical problems compared to outpatients. However, to the best of our knowledge, there has been no report focusing on inpatients with movement disorders. Therefore, the aim of the current study is to investigate the characteristic features of inpatients presenting with movement disorders that may provide useful information to general neurologists as well as nonneurological doctors.
MATERIALS & METHODS
Patient selection
This study was performed at Korea University Guro Hospital, a 1074-bed teaching hospital in Seoul, Korea. From January 2013 to December 2014, a total of six members worked in the department of neurology. Among them, four worked in the hospital as movement disorder specialists (S-B.K and K-Y.K in 2013 and 2014; S-M.L in 2013; H.M.L in 2014). Patients were retrospectively selected from the medical records of all inpatient neurological consultations. We selected inpatients who were referred with a primary complaint of movement disorder as well as patients referred to movement disorder specialists assigned to the Parkinson’s disease Centre. We excluded consultations for an adverse effect of medications of inpatients with movement disorders or a situation in the emergency room. Each inpatient evaluation consisted of a medical interview, neurologic examination, and a screening for secondary etiology, including drug-associated adverse effects or metabolic problems such as renal insufficiency. Each movement disorder specialist occasionally discussed difficult cases with the chief professor (S-B.K) if the consultation was neither concluded nor resolved clearly. Movement disorders were diagnosed according to the appropriate established criteria for Parkinson’s disease (PD) [3], essential tremor (ET) [4], and dementia with Lewy bodies (DLB) [5]. For tremor disorders, the consensus statement of the Movement Disorder Society on tremor was also consulted [6]. Periodic limb movement disorder (PLMD) was independently diagnosed according to the clinical history and phenomenology in response to medication [7], since most inpatients could not be tested using polysomnography. The present study protocol was reviewed and approved by the institutional review board of Korea University Guro Hospital (IRB: KUGH15159). All procedures performed were carried out in accordance with national law and the Declaration of Helsinki of 1964 (in its present revised form). Informed consent was not required since the current study was a retrospective study.
Clinical features of the inpatients with involuntary movement
In accordance with the protocol, inpatient medical records were reviewed by one physician (K-Y.K) to obtain the patient’s demographic data and clinical features. The consultations were clinician-dependent, and the following clinical characteristics were extracted and subcategorized: 1) mode of onset, 2) the referral symptom described by physicians or surgeons, 3) the representative movement pattern described by movement disorder specialists, 4) the diagnosis of movement disorder, and 5) whether the symptom started before or after admission in the hospital to aid in the diagnosis of the inpatient’s movement disorder. Furthermore, clinical characteristics such as mode of onset and movement disorder diagnosis were defined and/or subcategorized. According to the initial onset time of movement symptoms, the mode of onset was defined as acute (within several days), subacute (within several weeks), and chronic (from several months to years). Movement disorder diagnosis included toxic/metabolic-caused movement disorder (T/MCMD), PD, ET, benign tremor such as benign enhanced physiologic tremor or benign tremulous parkinsonism, PLMD, other rare movement disorders [hydrocephalus, DLB, or Huntington’s disease (HD)], neuromusculoskeletal problem, senile/nonspecific, and uncertain/undiagnosed.
Data analysis
Data analyses including numerical and categorical variables were performed with Microsoft Excel and SPSS version 20.0 (IBM Corp., Armonk, NY, USA).
RESULTS
Patient demographics
During the study period, a total of 3,774 in-hospital consultations, including 292 consultations (7.7%) primarily related to movement disorder, were conducted by all members of the hospital’s department of neurology. The 292 consultations were from 202 patients and were performed by movement disorder specialists. The demographics are shown in Table 1. Out of 202 inpatients, 111 were female (55%). The mean age ± SD was 70.7 ± 11.8 years (range of 17 to 94). Common referral doctors were from nonneurological medical departments (64.4%). The mean number ± SD of comorbidities was 2.4 ± 1.2, and the most common comorbid disease was hypertension (50.4%), followed by diabetes mellitus (32.2%), and musculoskeletal problems (26.7%). Moreover, serious medical problems, including respiratory disorders (22.3%), renal insufficiency (19.3%), and malignancy (17.3%), were relatively common.
Symptoms referred for neurological consultation
The presenting symptoms of inpatients are summarized in Table 2. The most common symptoms described by referring clinicians were tremor or tremor-like phenomenon (56.9%), followed by just ‘parkinsonism’ (16.8%), and gait disturbance (8.9%). In addition, the overall clinical features evaluated by movement disorder specialists are summarized in Table 3. The main features included parkinsonism (29.7%), myoclonus (28.2%), and tremor (23.8%).
Disease category of movement disorders in inpatients
The most common disorder diagnosed was T/MCMD (35%), followed by PD (16%), uncertain or undiagnosed (14%), other movement disorders, e.g., HD and hydrocephalus (13%), ET (6%), PLMD (6%), neuromusculoskeletal problem (5%), benign tremor (3%), and senile or nonspecific (2%) (Figure 1).
The disorders were subcategorized according to the mode of onset (Figure 2). The acute movement disorders (n = 47) were predominantly T/MCMD (68%), undiagnosed/uncertain (13%), other movement disorders (7%), benign tremor (4%), ET (2%), PD (2%), neuromusculoskeletal problem (2%), and senile/nonspecific (2%). The subacute movement disorders (n = 58) were T/MCMD (46%), other movement disorders (18%), undiagnosed/uncertain (16%), neuromusculoskeletal problem (9%), PD (5%), ET (2%), PLMD (2%), and senile/nonspecific (2%). The disease categories of the chronic movement disorders (n = 91) were a mix of PD (31%), other movement disorders (14%), T/MCMD (13%), ET (12%), PLMD (12%), undiagnosed/uncertain (10%), benign tremor (4%), neuromusculoskeletal problem (3%), and senile/nonspecific (1%). Six out of 202 patients were uncertain for the mode of onset.
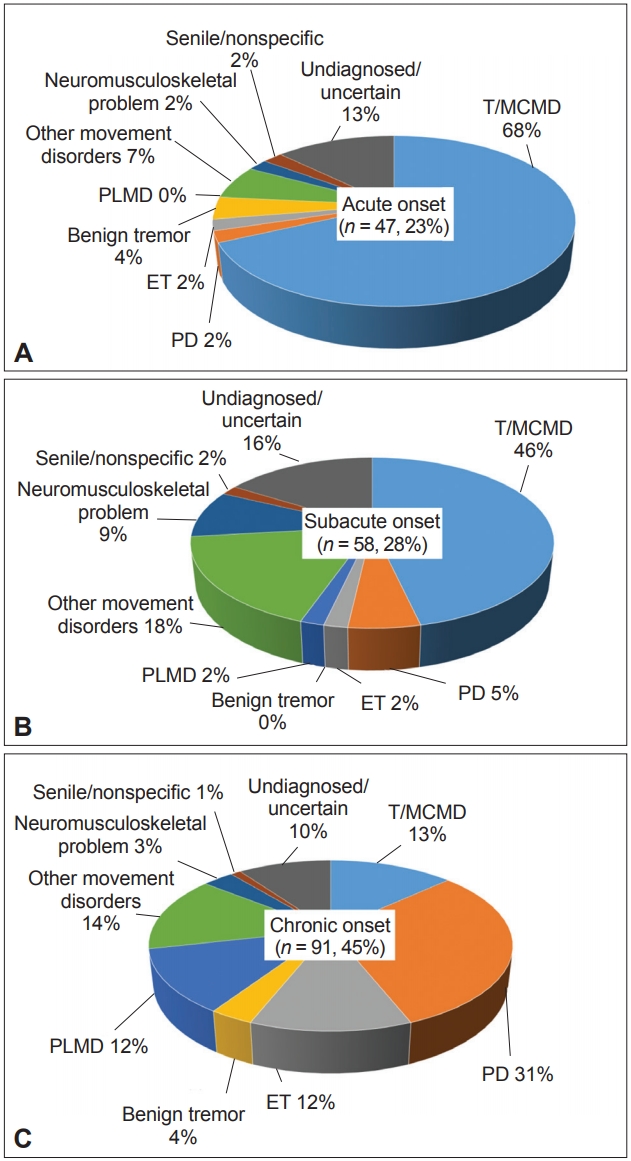
Prevalence of disease categories according to the mode of onset of movement disorders. Acute (A), subacute (B), and chronic (C) onset. T/MCMD: toxic/metabolic-caused movement disorder, PD: Parkinson’s disease, ET: essential tremor, PLMD: periodic limb movement disorder.
In addition, we performed an analysis of the subcategory of referred symptoms to determine their diagnosis by the movement disorder specialist. Tremor or tremor-like movement was the referral symptom most frequently consulted in the hospital. Patients with tremor-like symptoms (regarded as 100%) were diagnosed with T/MCMD (44.3%), uncertain (14.8%), ET (11.3%), PLMD (10.4%), other movement disorders (7%), PD (5.2%), benign tremor (4.3%), senile/nonspecific (1.7%), and neuromusculoskeletal problems (0.9%). The second most common referred symptom was parkinsonism. Patients with parkinsonism (summed as 100%) were diagnosed with PD (61.8%), T/MCMD (17.6%), uncertain or undiagnosed (14.7%), and two cases with other movement disorders of DLB (5.9%).
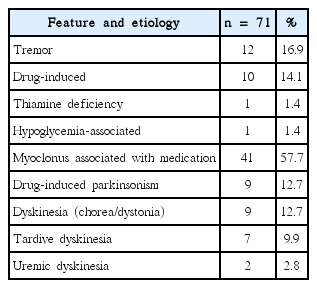
A post hoc analysis for toxic/metabolic-caused movement disorder
Since the most diagnosed disease category was T/MCMD, we analyzed the main movement symptoms as well as the main etiology in detail for T/MCMD in Table 4. As a result, we found that the crucial etiology was drug-induced movement disorder (94.4%) for T/MCMD, which breaks down to myoclonus (57.7%), tremor (14.1%), parkinsonism (12.7%), and dyskinesia (9.9%). In contrast, only 4.2% of cases (1.4% with hypoglycemia and 2.8% with uremia) were provoked only by metabolic causes.
DISCUSSION
This study focused on the clinical features of movement disorders in patients admitted during a 2-year period at nonneurological departments in a tertiary care university hospital. Previously, researchers have investigated outpatients attending movement disorder clinics and have revealed that the most common diagnosis is PD (59%) [8], and moreover, the diagnosis of PD has been gradually increasing [9]. Other investigators focused solely on patients with secondary movement disorders [10] or patients with movement disorders in the emergency department [11]. In addition, there have been studies demonstrating a pattern of overall neurological disorders for patients in the hospital [12-15] or in the medical intensive care unit [2]. However, to our knowledge, no analysis of patients with movement disorders from all nonneurological departments has been conducted.
The majority of the patients were very old with a mean age of 70.7 years and were admitted due to severe illness at other departments in the hospital, implying that the underlying medical condition of the patients could be fatal or serious. This suggests that our study might represent a pattern of movement disorders in elderly patients with relatively poor medical conditions.
Previous studies have revealed that the frequency of movement disorder consultations ranges from 4.9% to 6.5% among all neurologic consultations performed in the hospital [13-15]. In line with the literature, our study showed that movement disorder consultations rated 7.7% of all neurological referrals. However, Wenning et al. [16] (cohort study with an elderly population) reported a prevalence of movement disorders of 28%. This difference might be due to differences in the study protocol. In the former studies (consultation studies), patients were referred to specialists due to a medical need arising from a serious symptom, whereas in the latter study (cohort study), all participants underwent the screening protocol. In addition, Yoon et al. [11] showed that of the patients presenting with neurological problems in the emergency room, 2.3% of them had movement disorders.
Until now, there has been no report on the detailed characteristics or patterns of movement disorders in hospitalized patients. In patients from different hospital departments, our study showed that T/MCMD was the most common disorder, especially within the categories of acute and subacute onset. In addition, we found that the most frequent referral symptom was tremor-like movement, the majority of which was caused by T/MCMD. Moreover, almost all of the cases T/MCMD were attributed to drug-induced adverse effects rather than metabolic disorders. In line with our study, Yoon et al. [11] reported that druginduced movement disorders, including parkinsonism/myoclonus/dystonia/tremor, were the most common movement disorders (63.8%) observed in the emergency room. Overall, these findings suggest that clinicians in hospitals must pay careful attention to the medications taken by their patients as well as any underlying medical problems. However, we were unable to identify the exact drug causing T/MCMD, since 1) many patients had renal and/or hepatic failure in addition to taking a considerable number of drugs (i.e., a couple of candidate drugs to induce T/MCMD), suggesting that it was very difficult to identify only one drug responsible for drug-induced toxic effects and serious metabolic problems, including hepatic or renal insufficiency; 2) our consultation should have provided a prompt resolution to the inpatient’s referral symptom instead of having enough time to confirm an exact cause for the referred movement disorder; and 3) thus, we often advised the immediate discontinuation of all possible candidate drugs. We could deduce that this failure to identify the responsible drug might reflect the real clinical situation of inpatient consultation.
The current study has several limitations. First, the study was retrospective, and the protocol may have been insufficient in removing bias inherent to the design. However, the study utilized a standardized systematic approach to patient selection, and one physician followed an established protocol to evaluate the medical records of each patient. Second, we only reviewed neurological consultations conducted by movement specialists not only to increase the diagnostic accuracy but also to evaluate the details of the movement disorders. Inevitably, some consultations of inpatients with movement disorders referred to nonmovement disorder specialists were not assessed. Third, T/MCMD could not be investigated in detail to determine the etiologic medication or metabolic problem, as described previously. A more well-designed prospective study is required to address this issue. Fourth, some consultations may be made simply to inform a movement disorder professor about the admission of patients who had been followed up by the professor. These cases could be a source of biased results. Fifth, the study was conducted in a single hospital, implying that our observations could reflect a situation specific to our hospital. Thus, our results need to be interpreted with caution. Moreover, we could neither compare our results with any previous data, nor draw any consensus or conclusion for inpatient consultation of movement disorders since there has been no previous study to address this issue. The current study should be regarded as a pilot study, and more well-designed multicenter studies are needed to uncover the real clinical pattern of inpatients with movement disorders.
In conclusion, our data showed that a substantial portion of patients in the hospital could have various movement disorders. The current study revealed a characteristic pattern of symptoms and disease categories of movement disorders encountered in nonneurologic departments.
Notes
Conflicts of Interest
The authors have no financial conflicts of interest.
Acknowledgements
This work was partially supported by the Soonchunhyang University Research Fund.