Articles
- Page Path
- HOME > J Mov Disord > Volume 15(1); 2022 > Article
-
Brief communication
Current Status of Telemedicine for Parkinson’s Disease in Japan: A Single-Center Cross-Sectional Questionnaire Survey -
Mayuko Ogawa1,2
 , Genko Oyama1,2,3,4
, Genko Oyama1,2,3,4 , Satoko Sekimoto1
, Satoko Sekimoto1 , Taku Hatano1,2,4
, Taku Hatano1,2,4 , Nobutaka Hattori1,2,3,4
, Nobutaka Hattori1,2,3,4
-
Journal of Movement Disorders 2022;15(1):58-61.
DOI: https://doi.org/10.14802/jmd.21096
Published online: December 24, 2021
1Department of Neurology, Juntendo University School of Medicine, Tokyo, Japan
2Department of Neurodegenerative and Demented Disorders, Juntendo University School of Medicine, Tokyo, Japan
3Department of Home Medical Care System based on Information and Communication Technology, Juntendo University School of Medicine, Tokyo, Japan
4Department of Drug Development for Parkinson’s Disease, Juntendo University School of Medicine, Tokyo, Japan
- Corresponding author: Genko Oyama, MD, PhD, FAAN Department of Neurology, Juntendo University School of Medicine, 2-1-1 Hongo, Bunkyo-Ku, Tokyo 113-8421, Japan / Tel: +81-3-3813-3111 / Fax: +81-3-5800-0547 / E-mail: g_oyama@juntendo.ac.jp
Copyright © 2022 The Korean Movement Disorder Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objective
- Using telemedicine is a way to improve the accessibility of specialists for patients with Parkinson’s disease (PD); however, it is not widely used in Japan. We investigated the efficacy of telemedicine in PD by using a single-center cross-sectional questionnaire survey.
-
Methods
- We sent a questionnaire to patients who agreed to participate from among 52 patients with PD who had used telemedicine services at Juntendo University Hospital from October 2017 to November 2018. Caregivers were asked to respond to one question separately.
-
Results
- A total of 38 patients responded to the questionnaire. Most patients were satisfied with the telemedicine consultation (7.8 ± 1.9), reporting that it was effective in reducing their travel burden. Twenty-one patients attended a telemedicine consultation with their caregivers, and their satisfaction was high (8.4 ± 1.8).
-
Conclusion
- In a specific cohort in Japan, patients with PD and their caregivers were mostly satisfied with the telemedicine service.
- Patients
- The inclusion criteria were 1) persons with PD (fulfilling the United Kingdom Parkinson’s Disease Society Brain Bank Criteria), 2) making regular visits to Juntendo University Hospital, 3) and using our telemedicine service (Supplementary Material and Supplementary Figure 1 in the online-only Data Supplement) at least once during the first year of service initiation (from October 2017 to November 2018), 4) who were over 20-year-old, and 5) provided written consent after the research was completely explained.
- Study protocol
- The institutional review boards at Juntendo University Hospital approved the research protocol (#18-295) and the consent forms. This study was conducted in accordance with the ethical standards of the Declaration of Helsinki. We conducted a cross-sectional, questionnaire survey with 10 questions (Table 1). After explaining the details of the study by telephone, we sent the questionnaire and consent form to the patients’ homes. Patients who agreed to participate returned the written consent form and completed questionnaire. If the patient had a caregiver, the caregiver could help to fill out the questionnaire and respond to one question about how useful the system was for them. The responses were numerically rated from 0 (lowest) to 10 (highest). We also conducted a retrospective chart review of the clinical characteristics, including age, sex, disease duration, diagnosis, frequency of regular hospital visits, telemedicine, and adverse events. The travel expenses were calculated from patient-reported transportation using Navitaime (https://www.navitime.co.jp/). As this was an exploratory study, descriptive statistics were performed. The Pearson correlation coefficient was used to evaluate the correlation between satisfaction and clinical information.
MATERIALS & METHODS
- Among the 52 patients with PD who used telemedicine services, we sent a questionnaire to 46 patients who agreed to participate in the study (six patients declined). A total of 38 patients (15 males and 23 females) responded to the questionnaire (response rate: 82.6%). Their average age was 64.5 ± 9.3 (range: 39–78) years old. Their average disease duration was 10.1 ± 4.6 years.
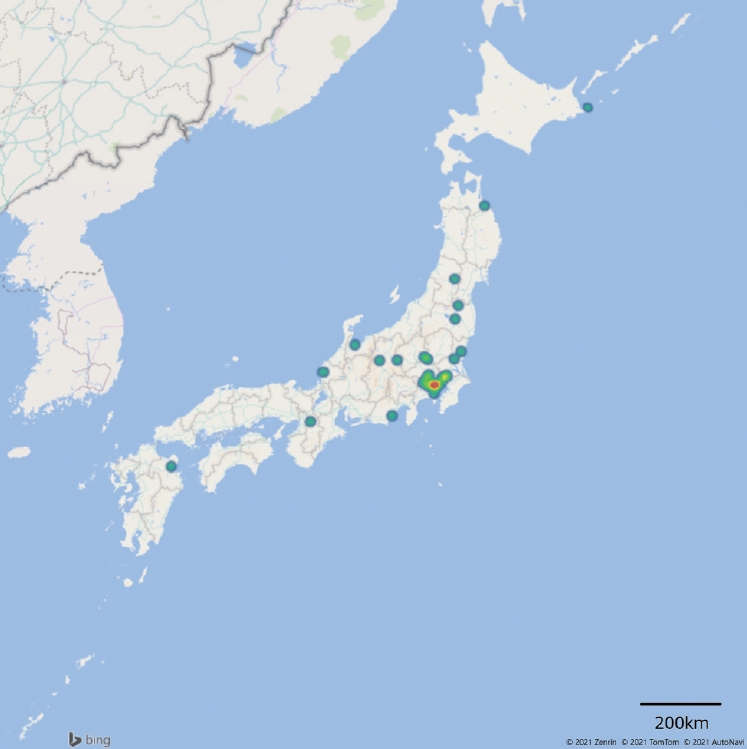
- Figure 1 shows the geographic distribution of patients who participated in this study. Although patients were from all over Japan, most lived in Tokyo and the surrounding area. The average travel time to our hospital was 136.8 ± 69.6 minutes. The transportation methods included taxis or the patients’ own cars (n = 31), trains (n = 28), airplanes (n = 4), or a combination of these. Five patients had to stay at a hotel or a relative’s house near the hospital. Twenty-seven (71%) patients visited the hospital with their caregivers, including their spouse (n = 22), children (n = 7), and relatives (n = 1). The cost of round-trip transportation was ¥18,531 ± ¥23,256 ($178.1 ± $223.6, at a rate of $1 = ¥104). If the patients needed a caregiver, the additional transportation cost was ¥27,189 ± ¥40,419 ($261.4 ± $388.6). If they needed to stay at a hotel for one night, the additional cost was ¥17,593 ± ¥18,189 ($169.1 ± $174.8).
- During telemedicine visits, 21 patients (55.3%) attended with their caregivers. The caregivers included the patient’s spouse (n = 16), children (n = 5), relatives (n = 1), and friends (n = 1). Most (84.2%) patients had a Wi-Fi connection. The average intervals between telemedicine consultations and face-to-face visits were 63.8 ± 26.2 days and 77.0 ± 31.5 days, respectively. The median number of telemedicine and in-person visits during the research period were 5 (interquartile range [IQR]: 3–6) and 5.5 (IQR: 3–7), respectively. Most patients had one telemedicine visit for every one or two in-person visits (telemedicine/in person=1.1 ± 0.9).
- Table 1 shows the results of the questionnaire. In general, both patients and caregivers gave high scores for their satisfaction with the telemedicine system. In particular, patients gave the highest scores for the reduction in their travel burden. There was no significant correlation between patients’ average satisfaction score and their age (r = -2.84, p = 0.84) or disease duration (r = 0.05, p = 0.78). No adverse events were observed.
RESULTS
- Our results showed that patients were satisfied with telemedicine using an iPad (Apple Inc.) and reported that it was effective in reducing their travel burden. This study also showed high satisfaction with telemedicine via an iPad in the treatment of PD, which is in line with the results of our previous pilot study [4].
- Although previous studies have reported high patient satisfaction with telemedicine using laptop or desktop computers and built-in carts [8-12], there are multiple choices for devices for telemedicine, such as smartphones, tablets, desktops, and laptops [6,7]. In particular, mobile devices that can change the camera angle may be useful for adequately capturing images during examinations. Smartphones as well as tablets can be used in telemedicine, but the resolution of tablets may be better for motor evaluation during examinations. Based on our experience, a Wi-Fi connection is required for adequate image and time resolution.
- Reducing travel burden and cost is the predominant benefit of telemedicine. Indeed, the expense of the telemedicine system is recovered if the travel cost is higher than ¥7,000 when patients use telemedicine visits every other month between regular visits. Most patients reported that telemedicine consultations were more useful than regular in-person visits and that this promoted efficient communication with a doctor, although specific points such as the effect of a lack of in-person meetings with physicians and the quality of care were not compared in this survey. Increasing the likelihood of being able to communicate with a doctor may reduce anxiety. Furthermore, communicating with doctors in a relaxed atmosphere may be helpful for efficient communication. More of the patient’s time set aside for visiting the hospital can be spent actually seeing a doctor and discussing their problems [13].
- In contrast, symptom stabilization was not enhanced by telemedicine, although it was comparable to that achieved through regular face-to-face visits. In general, both patients and caregivers were satisfied with the usefulness of the telemedicine system. In our preliminary questionnaire survey, the doctors also reported high satisfaction with telemedicine visits, although they did not agree that telemedicine was superior to face-to-face visits. They also did not agree that telemedicine reduced the doctor’s burden (Supplemental Table 1 in the online-only Data Supplement).
- In Japan, telemedicine has been covered by national insurance in cases that fulfill certain requirements since April 2018. However, telemedicine has not been popular, probably because of the limited number of cases that meet the requirements and because its amount of the insurance coverage is lower than that of a regular clinic visit. The requirements are that the patient has a chronic disease, the patient is attending a follow-up visit at least 6 months before the first online visit, the patient must attend face-to-face visits at least every 3 months, and the patient must have emergency access to the hospital within 30 minutes. These regulations have been tentatively expanded since April 10, 2020, due to the COVID-19 pandemic. As such, telemedicine visits using any device, including telephones, are now allowed for any disease, even for new patients. However, even under such conditions, the number of telemedicine consultations is still limited compared to that of regular visits and telephone consultations (Supplemental Figure 2 in the online-only Data Supplement), in contrast to the rapid expansion of telemedicine use worldwide after the pandemic [14-16]. Because patients are increasingly open to the idea of telemedicine due to the pandemic [17], the doctor’s burden and lower compensation from telemedicine compared to that from face-to-face visits might be a major barrier.
- In conclusion, telemedicine using tablets provides high satisfaction for patients with PD and their caregivers, reducing the travel burden and cost. Telemedicine may be an efficient alternative to face-to-face visits, although it precludes examinations and procedures that require physical contact. The limitations of the present study include its design and the small number of patients. In addition, the cohorts of our study may be early adopters and may not represent the general Japanese population; therefore, selection bias should be considered. Although this study is the first to elucidate real-world data in Japan, more studies are needed to develop a valuable and sustainable telemedicine system for patients with PD in the postpandemic era.
DISCUSSION
Supplementary Materials
Supplementary Table 1.
Supplementary Figure 1.
Supplementary Figure 2.
-
Conflicts of Interest
Department of Neurodegenerative and Demented Disorders is a joint-research course supported by GLORY LTD, Kirin Company LTD, Mitsubishi UFJ Lease & Finance Company LTD. The Department of Home Medical Care System based on Information and Communication Technology is a joint research course supported by Sunwels Co., Ltd. The Department of Drug Development for Parkinson’s Disease, Juntendo University Faculty of Medicine is a course supported by Ohara Pharmaceutical Co., Ltd. and PARKINSON Laboratories Co., Ltd. Dr. Oyama has received speaker honoraria from Medtronic, Boston Scientific, Otsuka Pharmaceutical Co. Ltd., Sumitomo Dainippon Pharma Co. Ltd., Eisai Co., Ltd., Takeda Pharmaceutical Company LTD., Kyowa Hakko Kirin Co. Ltd., and AbbVie, Inc. Dr. Hattori received speaker honoraria from AbbVie GK, EA Pharma, Eisai Co., Ltd., Otsuka Pharmaceutical Co., Ltd., Ono Pharmaceutical Co., Ltd., OHARA Pharmaceutical Co., Ltd., Kyowa Kirin Co., Ltd., Senju Pharmaceutical Co., Ltd., Sumitomo Dainippon Pharma Co., Ltd., Takeda Pharma Co., Ltd., Medtronic, Inc., and Novartis Pharma K.K. All of these have no concerning conflicts of interest with this manuscript.
-
Funding Statement
This study was partially supported by grants from the Japan Society for the Promotion of Science, Grants-in-Aid for Scientific Research (C) (#21K12711) and Grants-in Aid from the Research Committee of CNS Degenerative Diseases; Research on Policy Planning and Evaluation for Rare and Intractable Diseases; Health, Labour and Welfare Sciences Research Grants; and the Ministry of Health, Labour and Welfare, Japan (20FC1049).
-
Author Contributions
Conceptualization: Genko Oyama, Mayuko Ogawa, Satoko Sekimoto. Data curation: Mayuko Ogawa, Genko Oyama. Formal analysis: Mayuko Ogawa, Genko Oyama. Funding acquisition: Genko Oyama, Nobutaka Hattori. Investigation: Mayuko Ogawa, Genko Oyama. Methodology: Mayuko Ogawa, Genko Oyama, Satoko Sekimoto. Project administration: Genko Oyama. Resources: Genko Oyama. Software: Genko Oyama. Supervision: Genko Oyama, Taku Hatano, Nobutaka Hattori. Writing—original draft: Mayuko Ogawa, Genko Oyama. Writing—review & editing: Satoko Sekimoto, Taku Hatano, Genko Oyama, Nobutaka Hattori.
Notes

- 1. Obeso JA, Stamelou M, Goetz CG, Poewe W, Lang AE, Weintraub D, et al. Past, present, and future of Parkinson’s disease: a special essay on the 200th Anniversary of the Shaking Palsy. Mov Disord 2017;32:1264–1310.ArticlePubMedPMC
- 2. Moriwaka F, Tashiro K, Itoh K, Honma S, Okumura H, Kikuchi S, et al. Prevalence of Parkinson’s disease in Hokkaido, the northernmost island of Japan. Intern Med 1996;35:276–279.ArticlePubMed
- 3. Poewe W, Seppi K, Tanner CM, Halliday GM, Brundin P, Volkmann J, et al. Parkinson disease. Nat Rev Dis Primers 2017;3:17013.ArticlePubMed
- 4. Sekimoto S, Oyama G, Hatano T, Sasaki F, Nakamura R, Jo T, et al. A randomized crossover pilot study of telemedicine delivered via iPads in Parkinson’s disease. Parkinsons Dis 2019;2019:9403295.ArticlePubMedPMC
- 5. Kadoya Y, Hara M, Takahari K, Ishida Y, Tamaki M. Disease control status and safety of telemedicine in patients with lifestyle diseases-A multicenter prospective observational study in Japan. Circ Rep 2020;2:351–356.ArticlePubMedPMC
- 6. Achey M, Aldred JL, Aljehani N, Bloem BR, Biglan KM, Chan P, et al. The past, present, and future of telemedicine for Parkinson’s disease. Mov Disord 2014;29:871–883.ArticlePubMed
- 7. De Marchi F, Contaldi E, Magistrelli L, Cantello R, Comi C, Mazzini L. Telehealth in neurodegenerative diseases: opportunities and challenges for patients and physicians. Brain Sci 2021;11:237.ArticlePubMedPMC
- 8. Fincher L, Ward C, Dawkins V, Magee V, Willson P. Using telehealth to educate Parkinson’s disease patients about complicated medication regimens. J Gerontol Nurs 2009;35:16–24.Article
- 9. Venkataraman V, Donohue SJ, Biglan KM, Wicks P, Dorsey ER. Virtual visits for Parkinson disease: a case series. Neurol Clin Pract 2014;4:146–152.ArticlePubMedPMC
- 10. Dorsey ER, Wagner JD, Bull MT, Rizzieri A, Grischkan J, Achey MA, et al. Feasibility of virtual research visits in fox trial finder. J Parkinsons Dis 2015;5:505–515.ArticlePubMedPMC
- 11. Wilkinson JR, Spindler M, Wood SM, Marcus SC, Weintraub D, Morley JF, et al. High patient satisfaction with telehealth in Parkinson disease: a randomized controlled study. Neurol Clin Pract 2016;6:241–251.ArticlePubMedPMC
- 12. Barbour PJ, Arroyo J, High S, Fichera LB, Staska-Pier MM, McMahon MK. Telehealth for patients with Parkinson’s disease: delivering efficient and sustainable long-term care. Hosp Pract (1995) 2016;44:92–97.ArticlePubMed
- 13. Dorsey ER, Venkataraman V, Grana MJ, Bull MT, George BP, Boyd CM, et al. Randomized controlled clinical trial of “virtual house calls” for Parkinson disease. JAMA Neurol 2013;70:565–570.ArticlePubMedPMC
- 14. Webster P. Virtual health care in the era of COVID-19. Lancet 2020;395:1180–1181.ArticlePubMedPMC
- 15. Shalash A, Spindler M, Cubo E. Global perspective on telemedicine for Parkinson’s disease. J Parkinsons Dis 2021;11:S11–S18.ArticlePubMedPMC
- 16. Hassan A, Mari Z, Gatto EM, Cardozo A, Youn J, Okubadejo N, et al. Global survey on telemedicine utilization for movement disorders during the COVID‐19 pandemic. Mov Disord 2020;35:1701–1711.ArticlePubMedPMC
- 17. Kurihara K, Nagaki K, Inoue K, Yamamoto S, Mishima T, Fujioka S, et al. Attitudes toward telemedicine of patients with Parkinson’s disease during the COVID‐19 pandemic. Neurol Clin Neurosci 2021;9:77–82.Article
REFERENCES
Figure & Data
References
Citations

- A Survey of Perspectives on Telemedicine for Patients With Parkinson’s Disease
Jae Young Joo, Ji Young Yun, Young Eun Kim, Yu Jin Jung, Ryul Kim, Hui-Jun Yang, Woong-Woo Lee, Aryun Kim, Han-Joon Kim
Journal of Movement Disorders.2024; 17(1): 89. CrossRef - Expert teleconsultation involving patients and their primary neurologists for the management of multiple sclerosis in regions without specialists
Yusei Miyazaki, Shigehisa Ura, Kazuhiro Horiuchi, Takeshi Matsuoka, Hideki Houzen, Kazufumi Tsuzaka, Yuichi Makino, Manami Koshida, Genko Oyama, Chika Sato, Ryoji Naganuma, Itaru Amino, Sachiko Akimoto, Masaaki Niino, Naoya Minami, Eri Takahashi, Susumu O
Clinical and Experimental Neuroimmunology.2024;[Epub] CrossRef - Effects of LSVT-BIG via telerehabilitation on non-motor and motor symptoms and quality of life in Parkinson’s disease
Yasemin Ekmekyapar Fırat, Türkan Turgay, Selver Seval Soğan, Pınar Günel Karadeniz
Acta Neurologica Belgica.2023; 123(1): 207. CrossRef - A Narrative Review of Current Status and Future Perspective of Telemedicine for Parkinson's Disease, Dementia, and Intractable Neurological Diseases in Japan
GENKO OYAMA, MAYUKO OGAWA, SATOKO SEKIMOTO, TAKU HATANO, NOBUTAKA HATTORI
Juntendo Medical Journal.2023; 69(1): 14. CrossRef - A multicenter, prospective, observational study to assess the satisfaction of an integrated digital platform of online medical care and remote patient monitoring in Parkinson's disease
Makoto Shiraishi, Tsutomu Kamo, Ryuya Kumazawa, Naoshi Sasaki, Kenji Isahaya, Hisanao Akiyama, Yoshihiko Furusawa, Reiko Onodera, Jovelle Fernandez, Masaru Otsuka, Yoshihisa Yamano
Neurology and Clinical Neuroscience.2023; 11(3): 152. CrossRef - New era of artificial intelligence and machine learning-based detection, diagnosis, and therapeutics in Parkinson’s disease
Rohan Gupta, Smita Kumari, Anusha Senapati, Rashmi K. Ambasta, Pravir Kumar
Ageing Research Reviews.2023; 90: 102013. CrossRef - Feasibility study of Internet video-based speech-language activity for outpatients with primary progressive aphasia
Shinji Higashi, Yuko Koshibe, Takehiro Miyazaki, Ryohei Watanabe, Hanako Nakanome, Takeshi Inoue, Takashi Asada, Tetsuaki Arai, Kenjiro Ono
PLOS ONE.2023; 18(7): e0288468. CrossRef - Feasibility and efficacy of video-call speech therapy in patients with Parkinson's disease: A preliminary study
Hee Jin Chang, Jiae Kim, Jae Young Joo, Han-Joon Kim
Parkinsonism & Related Disorders.2023; 114: 105772. CrossRef - Perspectives on Telemedicine
彦光 大山, 信孝 服部
Iryou kikigaku (The Japanese journal of medical instrumentation).2022; 92(3): 331. CrossRef
Comments on this article
 KMDS
KMDS
 E-submission
E-submission
 PubReader
PubReader ePub Link
ePub Link Cite
Cite