Articles
- Page Path
- HOME > J Mov Disord > Volume 16(3); 2023 > Article
-
Letter to the editor
Gravitational syncope induced by rising elevators in a Parkinson’s disease patient -
Sun-Woo Sohn1
 , Dallah Yoo1,2
, Dallah Yoo1,2 , Tae-Beom Ahn1,2
, Tae-Beom Ahn1,2

-
Journal of Movement Disorders 2023;16(3):331-332.
DOI: https://doi.org/10.14802/jmd.23076
Published online: June 9, 2023
1Department of Neurology, Kyung Hee University Hospital, Seoul, Korea
2Department of Neurology, College of Medicine, Kyung Hee University, Seoul, Korea
- Corresponding author: Tae-Beom Ahn, MD, PhD Department of Neurology, Kyung Hee University Hospital, College of Medicine, Kyung Hee University, 23 Kyungheedae-ro, Dongdaemun-gu, Seoul 02447, Korea / Tel: +82-2-958-8448 / Fax: +82-2-958-8490 / E-mail: taebeom.ahn@khu.ac.kr
Copyright © 2023 The Korean Movement Disorder Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 800 Views
- 40 Download
- Dear Editor,
- Orthostatic hypotension (OH) is a common autonomic abnormality in patients with Parkinson’s disease (PD) [1]. General measures such as preventing dehydration or rising quickly after prolonged sitting or recumbency are underscored to prevent harmful events, including syncope, in addition to appropriate medical management. Herein, we report an unusual event leading to syncope related to OH, which could be added to the list of general warnings for PD patients with OH.
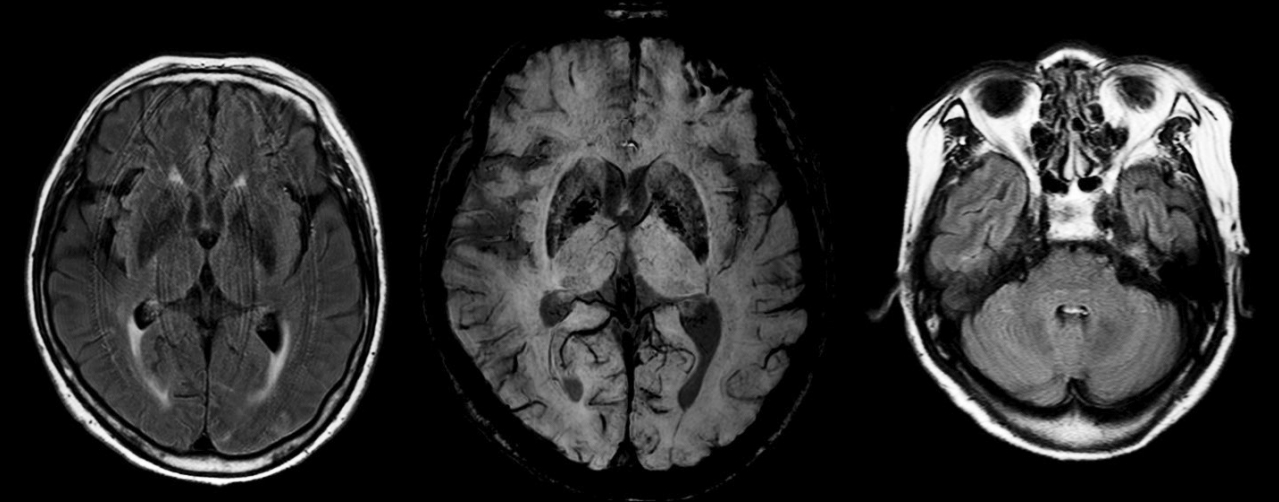
- A 66-year-old woman visited our hospital complaining of tremor and slowness. She had a brother with PD and a history of decreased bowel frequency, hyposmia, and parasomnia suggestive of rapid eye movement behavior disorder. Urinary incontinence was absent. A neurological examination showed bradykinesia, resting tremor, and preserved postural reflex. Deep tendon reflexes were normoactive. Cerebellar dysfunction was absent. A dopamine agonist and levodopa were effective for her parkinsonism. She started to experience wearing off, peak dose dyskinesia, and orthostatic dizziness after 3 years. Brain magnetic resonance imaging showed normal putamen and cerebellum volumes and no stenosis of the major intra- and extracranial arteries (Figure 1). Cardiac workups, including a chest X-ray, an electrocardiogram, and transthoracic echocardiography, were normal. The systolic blood pressure, diastolic blood pressure, and pulse rate were 106 mmHg, 66 mmHg, and 63 beats/min at baseline, and 69 mmHg, 40 mmHg, and 80 beats/min after 3 minutes of standing. Thus, the change in systolic blood pressure (dSBP) was -37 mmHg, in diastolic blood pressure was -26 mmHg, and in the heart rate (dHR) was +17 beats/minute (BPM) (dHR/dSBP = 0.45 BPM/mmHg) Afterward, she experienced increasing numbers of syncope events related to rapid positional changes along with visual hallucinations and cognitive impairment (MiniMental State Examination score = 17). At the age of 75 years, she had several episodes of syncope in an elevator only during upward acceleration. Her medications were levodopa 100 mg five times a day, pramipexole 0.75 mg QD, and rivastigmine 5 mg QD, which remained unchanged for 3 months before the syncope events in the elevator. She did not take any other medications that affected her blood pressure. One day, her family took video recordings of her video inside an elevator (Supplementary Video 1 in the online-only Data Supplement). Various drugs, such as fludrocortisone, midodrine, droxidopa, and pyridostigmine, were provided to treat OH, which was partially effective (droxidopa) or ineffective.
- The patient responded to dopaminergic medications with motor complications, which was compatible with the diagnosis of PD. Dizziness in an elevator has been described in a patient with multiple system atrophy (MSA), but syncope in an elevator has never been reported in MSA or PD patients [2]. Her syncope events in an elevator are the first reported in a PD patient with OH. All medications, such as levodopa, pramipexole, and rivastigmine, could be associated with OH, which had not been changed for 3 months before the occurrence of the syncope events in an elevator. Thus, the direct contribution of the drugs to the specific type of syncope may not be critical because of the poor temporal correlation between the change in medications and gravitational syncope. In an elevator, the upward acceleration of the elevator generates force toward the ground, augmenting the gravitational force. The combined force could hamper the blood rush to the brain, which might have resulted in syncope in this patient. More caution is needed in moving elevators in PD patients with severe OH.
Supplementary Material
Video 1.
-
Ethics Statement
This study was reviewed and approved by the Institute Review Board of Kyung Hee University Hospital (KHUH 2021-09-001). Informed consent was obtained for video footage.
-
Conflicts of Interest
The authors have no financial conflicts of interest.
-
Funding Statement
None
-
Author contributions
Conceptualization: Tae-Beom Ahn. Data curation: all authors. Investigation: all authors. Methodology: all authors. Project administration: Tae-Beom Ahn. Resources: Tae-Beom Ahn. Supervision: Tae-Beom Ahn. Visualization: Sun-Woo Sohn, Dallah Yoo. Writing—original draft: Sun-Woo Sohn, Dallah Yoo. Writing—review & editing: Dallah Yoo, Tae-Beom Ahn.
Notes
- 1. Velseboer DC, de Haan RJ, Wieling W, Goldstein DS, de Bie RM. Prevalence of orthostatic hypotension in Parkinson’s disease: a systematic review and meta-analysis. Parkinsonism Relat Disord 2011;17:724–729.ArticlePubMedPMC
- 2. Botticelli JT, Keelan MH Jr, Rosenbaum RF, Lange RL. Circulatory control in idiopathic orthostatic hypotension (Shy-Drager syndrome). Circulation 1968;38:870–879.ArticlePubMed
REFERENCES
Figure & Data
References
Citations

Comments on this article
 KMDS
KMDS
 E-submission
E-submission
 PubReader
PubReader ePub Link
ePub Link Cite
Cite

